Introduction
Although invasive mechanical ventilation (IMV) is a necessary treatment approach that has contributed to the survival of preterm infants with extremely low birth weight (ELBW) over the years, it is also associated with unsatisfactory clinical outcomes when used for prolonged periods, including bronchopulmonary dysplasia (BPD), retinopathy of prematurity (ROP) and neurological injuries. In addition, the risk for serious neurodevelopment impairment increases considerably for each additional week of IMV; therefore, it is highly recommended that weaning and discontinuation of IMV occur as soon as possible.1,2
Extubation failure is associated with higher morbidity and mortality rates in preterm infants; thus, the decision to extubate must be taken with great caution.3,4 Criteria for successful IMV weaning and extubation in the neonatal and pediatric populations remain inconsistent and not well established compared to an adult population, nor are there any reliable, validated tests for extubation readiness in this population. Usually, criteria vary according to each Neonatal Intensive Care Unit’s (NICU) practice.5–7 Currently, some research regarding predictive factors for successful extubation in the neonatal and pediatric population exists; however, most of the results have shown low precision and little benefit in identifying extubation failures.8,9
The present study aims to identify factors that may be crucial for extubation success in very low birth weight (VLBW) and ELBW preterm infants and investigate outcomes associated with extubation failure.
Methods
Study design and sample
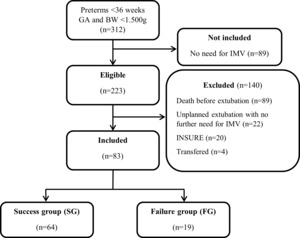
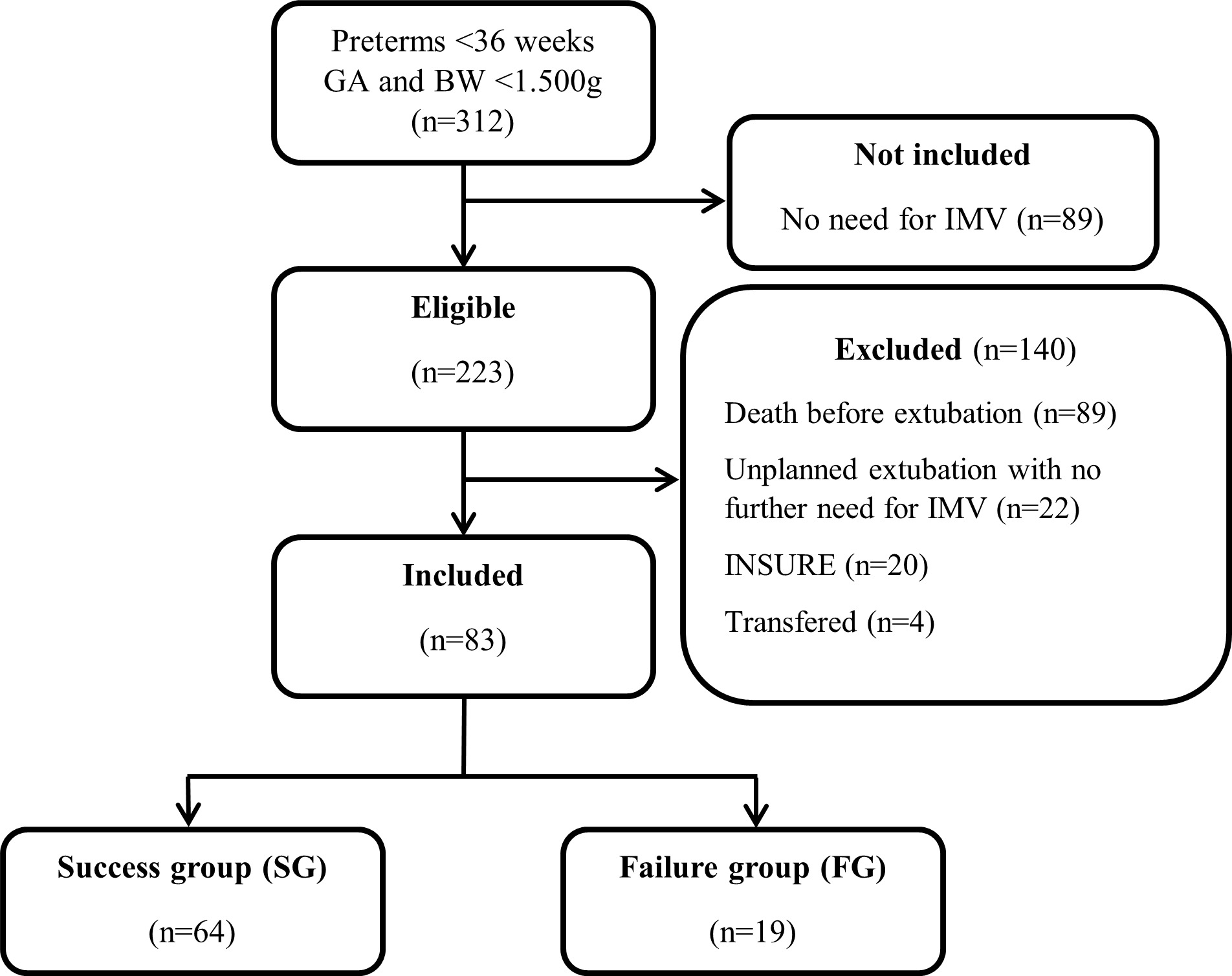
A retrospective, cohort, single-center study was conducted at the State University of Londrina–Brazi. All preterm born at <36 weeks postmenstrual age (PMA) and birth weight (BW) <1500 grams who underwent IMV during hospitalization between January 2015 and December 2018 were eligible. Infants who died before the extubation attempt, who underwent unplanned extubation and did not need to return to IMV after successful non-invasive post-extubation ventilation support, who got transferred to another institution before being discontinued from IMV, who got intubated briefly just for INSURE therapy (INtubation, SURfactant, Extubation) and infants whose data records were incomplete or not found were excluded. The study was approved by the Research Ethics Committee Involving Human Beings–State University of Londrina–Brazil (CAAE: 48415015.0.0000.5231).
Data collection
The following data were collected from patients’ data records: a) perinatal variables including gestational age (GA), BW, classification, gender, mode of delivery, 1 and 5 min Apgar scores, antenatal steroid and surfactant administration; b) initial ventilation variables including resuscitation in the delivery room, ventilatory parameters during transportation from the delivery room to the NICU, initial ventilatory parameters at NICU admission and after 24 hours of IMV; c) pre-extubation variables including caffeine and steroids administration, need for endotracheal tube (ET) replacement, unplanned extubations occurrence, PMA and weight at extubation, ventilatory parameters and blood gas variables right before extubation; d) post-extubation variables including first post-extubation respiratory support of choice, post-extubation blood gas variables, length of time on IMV, length of time on non-invasive ventilation (NIV)–continuous positive airway pressure (CPAP) and/or nasal intermittent positive pressure ventilation (NIPPV), and length of stay in NICU and hospital stay.
Successful extubation was defined as not requiring re-intubation during a pre-specified window of observation of 72 hours. Patients included in this study were allocated into the successful extubation group (SG) and the failed extubation group (FG). Infants under IMV were treated using the Dräger Babylog VN500 ventilator (Dräger, Lübeck, Germany).
Statistical analysis
Statistical analysis was performed using SPSS Statistics 22 (IBM Corp, Armonk, NY) and Graph Pad Prism 6.0 software (GraphPad Software Inc.; San Diego, California, USA). Data normality analysis was performed using the Shapiro-Wilk test, and data were described as percentages and mean ± standard deviation or median and interquartile range, depending on the normality test. Comparison of variables between groups was performed by Student’s t-test or Mann-Whitney test for continuous data, and proportion measurements were analyzed using the Chi-square test or Fisher’s exact test. Correlation between variables and duration of invasive mechanical ventilation was conducted using Pearson or Spearman rank correlation. Values 0.7-0.89 were considered strong, 0.5-0.69 reasonable, and 0.3-0.49 poor.10
To verify independent factors associated with extubation success, variables with significant differences between infants of the two groups which demonstrated association in a generalized linear mixed model (p<0.05) were included in a binary stepwise logistic regression model presented as odds ratio values and respective 95% confidence interval (95% CI) which indicated the associations’ magnitude. The adjusted logistic regression model included independent variables that showed an association of up to 20% extubation success (univariate model). Extubation success was set as a dependent variable. The statistical significance adopted was p<0.05.
Results
Between 2015 and 2018, 312 preterm babies with GA <36 weeks and BW <1500 grams were born and admitted to the NICU. Among 223 eligible infants, 140 were excluded, resulting in a final sample of 83 patients (Figure 1). No outborn babies were included.
Comparisons regarding perinatal variables between the two groups can be found in Table 1. There was a significant difference between them only regarding GA, BW and, consequently, weight classification.
There was no difference between the groups regarding resuscitation in the delivery room, ventilatory parameters during transportation from the delivery room to the NICU and initial ventilatory parameters set at NICU admission (Table 2). Most infants in both groups needed resuscitation in the delivery room. Most infants in the FG group were intubated while still in the delivery room.
FG infants had lower weight at extubation and, proportionally to SG, had more unplanned extubations and ET replacements. As for the ventilatory parameters right before extubation, SG needed lower FiO2. There was no difference concerning blood gas values. More information on the pre-extubation aspects is shown in Table 3.
NIPPV was the most used first post-extubation respiratory support of choice in both groups, as presented in Table 4. Post-extubation arterial partial pressure of carbon dioxide (PaCO2) and bicarbonate (HCO3-) values were higher in FG. Regarding variables during hospitalization, FG infants stayed a more extended time under IMV; length of stay in the NICU and overall hospital stay were also higher in that group.
In FG, a strong and negative correlation was found between IMV duration and GA (r=-0.81; p<0.0001); a reasonable and positive correlation between inspiratory pressure (Pinsp) during transportation, initial set Pinsp and initial set FiO2 with IMV duration (r=0.61, p=0.03; r=0.52, p=0.02 and r=0.54, p=0.01, respectively); a poor and positive correlation between initial set respiratory rate (RR) and IMV duration (r=0.48, p=0.04).
As for SG, a reasonable and positive correlation was found between HCO3- values both prior and post-extubation with IMV duration (r=0.6, p<0.0001 and r=0.63, p<0.0001, respectively); a poor and positive correlation between pre-extubation FiO2, pre and post-extubation PaCO2 with IMV duration (r=0.36, p=0.03; r=0.33, P=0.01 and r=0.26, p=0.02, respectively).
Statistically significant results of associated variables in the univariate analysis were inserted in the multivariate model (Table 5). Final logistic regression identified GA (OR 0.44; 95% CI 0.23, 0.85, p=0.01) and post-extubation PaCO2 (OR 1.1; 95% CI 1.0, 1.2, p=0.02) as extubation success predictors. The model was significant (X2 (9) 31.333, p<0.0001, R2 Nagelkerke=0.48) and correctly classified 85.4% of the cases.
Discussion
The purpose of the present cohort study was to identify factors that may be crucial for extubation success in VLBW and ELBW preterm infants and investigate outcomes associated with extubation failure by analyzing a series of factors that could predict extubation success in order to assist in the decision for the ideal moment of ET removal in these infants. The logistic regression analysis shows that higher GA and lower post-extubation PaCO2 were predictors of extubation success. Manley et al.11 analyzed pre and post-extubation data of 160 extremely preterm infants and, even considering a longer observation window for extubation success (168 hours after ET removal), also showed that GA and post-extubation PaCO2 predicted extubation success.
In clinical practice, arterial blood gas values are vital information to guide the decision to extubate extremely preterm infants.12 The current study showed that post-extubation PaCO2 was more significant as an extubation predictor than pre-extubation blood gas measures. There was no difference regarding Pinsp and RR adjusted at the moment immediately before extubation between the two groups. Since blood gas values strongly depend on these two ventilatory parameters, pre-extubation gasometric values were not appropriate to predict extubation success.
It is important to emphasize that, even though in the present study, we found post-extubation PaCO2 as an extubation success predictor, which is a variable representative of the moment after the primary outcome, this does not diminish its clinical relevance since the extubation process does not implicate in ET removal only, but it also involves all the aspects that take place within the specified period (72 hours, in this case) after the event (e.g., post-extubation NIV, the possibility of infections, the need for respiratory care). Closely observing post-extubation PaCO2 can possibly indicate an imminent rise in extubation failure, allowing the medical team to take effective measures to prevent it. For example, a better NIV adjustment (i.e., a more suitable NIV interface) and respiratory care optimization (e.g., airway clearance and lung expansion techniques). Re-intubation was considered if the baby presented increased work of breathing, severe apnea and bradycardia events and SpO2 <90% with FiO2 >0.5, indicating failure of NIV support.
Post-extubation arterial partial pressure of carbon dioxide (PaCO2) and bicarbonate (HCO3-) values were higher in FG. These higher values may be attributed to the fact that these babies experienced more respiratory distress, directly impacting gas exchange and, consequently, blood gases and acid-base balance.13
To date, there is still no consensus concerning the definition of extubation success in preterm infants. Therefore, for this study, we defined extubation success as not requiring reintubation after a specified 72 hour observation window because we understand that extrapolation of this time window to 120, or even 168 hours, could include cases of extubation failure whose causes would not be exclusively respiratory, deviating from the proposal of this study. Gupta et al.,13 faced with these definitions inconsistencies, analyzed predictive factors for extubation success in EPT infants using 72 and 120 hours as observation windows and obtained similar results in both analyses.
Extubation failure is defined as the requirement for re-intubation within a pre-specified observation period due to the inability to sustain spontaneous breathing. The rate of extubation failure in this study was 22.8%, mainly related to recurrent apneas and increased work of breathing, an outcome very similar to the Wang et al.14 study, which included 68 ELBW infants and considered extubation failure as the necessity to return to IMV within 168 hours, they observed an extubation failure rate of 23.5% primarily associated with apneas events, bradycardia and pulmonary hemorrhage. Dimitrou et al.15 and Kamlin et al.5 also presented extubation failure rates similar to this study, 19.4% and 22%, respectively.
Upon extubation, in this study, babies were usually placed on CPAP (PEEP 5-7 cmH2O) and minimum FiO2 necessary to maintain SpO2 levels between 91-95% or NIPPV (PIP 15-20 cmH2O, PEEP 5-7 cmH2O, inflation rates 20-40/minute and minimum FiO2 necessary to maintain SpO2 levels between 91-95%), depending on patient’s clinical characteristics. Weaning from CPAP and NIPPV was considered when the baby had PMA >32 weeks, no signs of increased work of breathing, no episodes of apnea or bradycardia and FiO2 21%. This strategy is in accordance with common practices applied in NICU services to prevent extubation failure.16
Compared to SG infants, FG infants had lower GA and BW, elements which can prove to be quite determinant not only for the occurrence of extubation failure but also for predicting mortality in ELBW infants.17,18 According to Hermeto et al.,17 lower GA was associated with higher rates of extubation failure due to greater pulmonary and muscular systems immaturity, which considerably impacts lung function and work of breathing.
A recent cohort study involving 312 preterm infants born with BW <1.250g found that higher GA, greater age at extubation, higher pre-extubation pH value and lower pre-extubation adjusted FiO2 are predictors for extubation success.13 Lower FiO2 and higher pH right before extubation may indicate better lung maturity and function, enough to favour spontaneous breathing. In our study, FG infants had lower weight and higher adjusted FiO2 at the time of extubation. Furthermore, these babies were older, which corresponds to Costa et al.'s19 findings that observed the greater the age at extubation, the greater the probability of extubation failure due to increased risk of complications such as bronchopulmonary dysplasia (BPD), hospital infection and lung injury ventilator-induced lung injury (VILI).
In this study, the unplanned extubation rate was 18%, with a higher proportion of these events in FG. This might be explained by the fact that these babies spent more on IMV, which inexorably increases the chances of unplanned extubations. A cohort study by Hatch et al.,20 which included 718 infants under IMV, found that between the first and fourth week of life, the risk for unplanned extubation increases by 36% each week and is associated with substantial damage such as clinical condition deterioration and cardiorespiratory arrest, besides a more extended hospital stay.
Proportionally, FG had more ET replacements (42.1%); this can be attributed to the fact that these infants were smaller (i.e., lower GA and BW) and consequently were initially intubated with a smaller diameter cannula. Furthermore, they were submitted to IMV for a longer time, which eventually required ET replacement for a larger size due to tube leakage increase as they grew. According to Mahmoud et al.,21 preterm ELBW infants mechanically ventilated for long periods have a greater risk for air leakage around the ET, mostly due to variations in body weight during hospitalization. Leaks greater than 40% can significantly compromise the delivery of adjusted targeted volume, impairing ventilation as a whole, hence the importance of proper endotracheal tube size placement in these babies according to their body weight.
Caffeine administration and its benefits for preterm infants have been widely investigated over the past two decades. It is routinely administered to extremely preterm neonates to prevent or treat apnea of prematurity.22–24 In our sample, 83% of the babies received caffeine before the first extubation attempt. Although it was not statistically significant, it is important to highlight the 17% difference in caffeine use between the two groups, considering that FG stayed longer under IMV. A large multicenter trial25 showed that caffeine administration in preterm infants born with BW between 500 and 1250 g was associated with a lower occurrence of BPD and faster IMV weaning.
As in previous studies,4,11,26 this study demonstrated that extubation failure occurrence is associated with longer IMV duration and hospital stay, which inexorably expose these patients to greater risks for unfavourable outcomes such as death or moderate/severe BPD as shown by Kaczmarek et al.27
This study has some limitations. First, as this is a cohort study with data from a single center, the generalizability of our findings might be limited. However, the clinical characteristics were similar to other, larger sample cohort studies.13,20 Also, it is noteworthy that the sample was unbalanced since this study had 64 infants in SG and 19 in FG, which might reflect the centre’s good practices regarding weaning and extubation. Another potential limitation is that this study focused only on the first event of extubation failure. It is known that ELBW infants may experience several episodes of extubation failure before finally leaving IMV successfully.
Despite the limitations, this was the first study to investigate the association between ventilatory support during transportation from the delivery room to NICU and initial adjusted ventilatory parameters with extubation success as well as with IMV duration, even though that was not the main purpose of this study. Furthermore, since data from only one center were used, the intubation, extubation, and re-intubation criteria had very little variability since the clinicians’ team followed institutional guidelines regarding these events, contributing to a more consistent clinical practice. Further studies following up on these patients, comparing long-term outcomes such as BPD, mortality, and neuropsychomotor development between FG and SG, might be important to support a likely impact of extubation failure occurrence over time.
Conclusion
In conclusion, we can state that GA and post-extubation PaCO2 were predictive variables for extubation success in VLBW and ELBW preterm infants. Those who experienced extubation failure had lower birth weights and higher adjusted FiO2 right before extubation.
Authorship
All the authors made substantial contributions to the work and declare that they have read and approved the manuscript.
Funding
The present study was partially funded by the following Brazilian agencies: Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES) - Finance Code 001. The study sponsors had no role in study design, data collection, data analysis and interpretation, the manuscript’s writing process and the decision to submit the manuscript for publication.
Conflict of Interest
The authors declare no conflicts of interest.
Ethical Approval
Ethical Requirement of Research Ethics Board approval for this project was approved by State University of Londrina – Brazil.
AI statement
The authors confirm that no generative AI or AI-assisted technology was used to generate content.