Introduction
In December 2019, a set of pneumonia cases, later proven to be caused by a new coronavirus (called “COVID-19”), appeared in Wuhan, Hubei Province, China.1 The World Health Organization (WHO) declared COVID-19 a pandemic in March 2020, raising an alert for an unprecedented public health emergency.2
Although most patients have a favourable outcome, approximately 5% have severe clinical manifestations with respiratory failure, septic shock and multiple organ failure.3 Prolonged intensive care unit (ICU) stay due to disease severity4,5 associated with intense inflammatory processes caused by COVID-19 infection6,7 may have potential effects on the musculoskeletal system, with decreased muscle mass and myopathies that predispose to muscle dysfunction that may contribute to loss of mobility, functional disability and decreased quality of life up to one year after hospital discharge.8
Thus, evaluating the patient’s functional status during the entire hospitalization, whether in the intensive care setting or not, becomes essential for advancing rehabilitation, which already starts during the hospitalization period. Several measuring instruments have been adapted to assess patients’ physical function in the ICU.9,10 All these assessment measures evaluate the physical function of patients, but only the Perme Score evaluates the barriers to mobilization in addition to patient-related factors.11,12
The Perme Score is an instrument that objectively measures the mobility status of patients admitted to the ICU. It comprises 15 items divided into seven categories, and the total Perme Score ranges from 0 to 32 points. Lower scores are associated with a lower level of mobility, and higher scores are associated with a higher level of mobility. In 2021, Timenetsky et al. used the Perme Score to describe the level of mobility of patients with COVID-19 admitted to the ICU and concluded that the level of mobility of patients was low on ICU admission and that most patients improved their level of mobility during the ICU stay.13 Continued assessment of functional status outside the intensive care setting ensures progress in the rehabilitation process. Thus, using the same instrument facilitates the comparison and evolution of the patient throughout hospitalization.
This study aims to evaluate the ability of the Perme Score to detect changes in the level of mobility of patients with COVID-19 outside the ICU and correlate the Perme Score value with length of stay.
Material and Methods
Type and location of the study
A retrospective cohort study was conducted in a private hospital’s inpatient unit medical clinic in São Paulo with data from February to October 2021.
Ethical Aspects
This study was submitted to and approved by the Ethics and Research Committee, and the Free and Informed Consent form was granted an exemption. This study is in accordance with the recently amended Declaration of Helsinki of 1975.
Data collection
Patients older than 18 years with a diagnosis of COVID-19 confirmed by reverse transcription polymerase chain reaction (RT–PCR) who were discharged from the ICU and remained in the inpatient units (IU) were included in the study.
All study data were retrieved from the electronic medical records by an independent research assistant from the Department of Clinical Medicine from February to October 2021. The data were tabulated in a REDCap database14 by the same research assistant, who did not participate as the author of this study. The data were made available to the authors completely anonymized.
Clinical variables
The variables collected included age, gender, length of stay in the ICU, date of intubation, date of extubation, time of invasive mechanical ventilation, date of hospitalization, date of hospitalization in the medical clinic, date of hospital discharge, Perme Score at admission to the inpatient unit and at hospital discharge, tracheostomy, tracheostomy date and tracheostomy decannulation date. In addition, the mobilization phases performed during physical therapy care ranging from 1 to 5 and following the institutional protocol were collected.15
The mobility level was evaluated using the “Perme Score of Mobility in the Intensive Care Unit” (Perme Score).11,12 This measurement instrument was developed and proposed to evaluate the mobility level of patients admitted to intensive care. It comprises 15 items divided into seven categories: mental status, potential mobility barriers, functional strength, bed mobility, transfers, gait, and endurance. The total score of the Perme ranges from 0 to 32 points (see Figure 1). The lowest scores are associated with a lower level of mobility, and the highest scores are associated with a higher level of mobility. The Perme Score was translated from the English language, adapted, and validated for use in the Portuguese language spoken in Brazil and is thus far considered the only ICU-specific measurement instrument to consider barriers to mobilization.12
In all comparisons, there was no evidence of a significant difference (p>0.05). *P values were obtained using the Mann–Whitney test. The score was calculated by the inpatient unit reference physiotherapists, who were trained to apply the score. The Perme assessment was performed on the day of admission of the patient to the inpatient unit and in the 24 hours before hospital discharge.
Statistical analysis
The data were described as absolute and relative frequencies for the categorical variables, medians and quartiles, and minimum and maximum values for the numerical variables. The distributions of the numerical variables were studied using histograms, boxplots, and the Shapiro-Wilk normality test.
Comparisons between patients older than 65 and up to 65 years old and in relation to gender regarding the Perme Score at entry and the variation of the Perme Score were performed using nonparametric Mann–Whitney tests. Values are expressed as medians (1st quartile; 3rd quartile), minimum and maximum values.
The Perme Scores were compared between the time at admission to the IU and at hospital discharge using a mixed linear model, considering the dependence between the applications of the instrument in the same patient. The results of the model are presented as estimated mean values, 95% confidence intervals (95%CI) and p values.
A logistic model was applied to investigate the relationship of the Perme Score on admission to the IU with the length of stay in the IU. The length of stay is dichotomized into long stay (more than seven days) or not (up to seven days). The results are presented as measures of effect, 95%CI and p values. The analyses were performed using the SPSS statistical package, considering a significance level of 5%.
Results
The database contained 89 records of patients with COVID-19 admitted to medical units after discharge from the ICU. Twenty patients were excluded because they did not have data on the Perme Score at admission to the IU and/or the date of hospital discharge.
A total of 69 patients were included, of whom almost 80% were male and had a mean age of 61.9 years (SD=12.5 years). The sample was quite homogeneous in relation to age, with 53.6% up to 65 years old and 46.4% over 65 years old. The demographic characteristics and length of hospital stay and ventilatory support are described in Table 1.
We investigated the differences between patients older than 65 years old and up to 65 years old and between men and women in relation to the Perme Score at admission to the IU and the variation in the Perme Score (difference between the Perme Score value at hospital discharge and upon admission to the IU). and the tests for the hypothesis of equality between the groups showed no evidence of differences (p> 0.05). See Figure 2.
The comparison of the Perme Score between admission to the IU and at hospital discharge shows significant variation (see Figure 3), with a mean increase of 7.3 points (95%CI: 5.7-8.8; p <0.001), with values of estimated mean of the Perme Score at admission to the inpatient unit of 17.5 (15.8; 19.3) and at hospital discharge of 24.8 (23.3; 26.3).
Considering the ceiling effect in the Perme Score, only one (1.4%) patient had a maximum score at the entrance and at the exit, and we observed a total of 12 (17.9%) patients with a maximum score among the 69 evaluated.
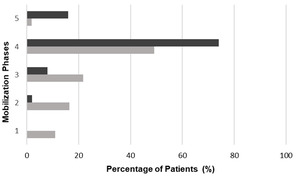
The mobilization phases performed during physical therapy are shown in Figure 3.
The logistic model that analyzed the association between the entry Perme Score value and length of hospital stay did not show a significant association with an effect measure and 95%CI 0.929 (0.861; 1.002; p=0.058).
Discussion
In this study, we demonstrated the mobility status of patients diagnosed with SARS-CoV-2 upon arrival at inpatient units, i.e., after discharge from the ICU, and their progression to hospital discharge using the Perme Score.
Our patients were predominantly male (79.7%), and the mean age was 61.9 years. Other authors found an average age similar to ours, approximately 60 years; however, in terms of sex, the distribution of these studies was 57%, 82% and 58%, respectively.13,16,17 In addition, our patients had a hospitalization time of more than 30 days, and almost half required tracheostomy, reinforcing the characteristics of critically ill patients exposed to potential risk factors for loss of functional mobility. Argenzioano et al., describing the characteristics of a thousand COVID-19 patients, found a length of hospital stay similar to that of our study, with an average of 23 days of hospitalization.18
Our study found no age or gender difference in the Perme Score values upon admission to the IU or in the Perme Score variation; however, the heterogeneous distribution of our sample in terms of sex (79.1% male) may have influenced this result. In contrast, Timenetsky identified a significant difference in age between patients who showed improvement in the Perme Score values in the ICU versus those who showed no improvement.13 The group with an improved Perme Score was younger, with a mean age of 62.5 years, compared to a mean age of 79.5 years in the group without improvement. This same study found no difference in relation to gender. A higher prevalence of frailty in females has been described in critically ill and non-critically ill populations.19,20 Therefore, assessing the impact of sex on the condition and clinical evolution must be very careful.
The impact on mobility as a consequence of musculoskeletal changes associated with myopathies and loss of muscle mass in critically ill patients has been described by several authors,4,21,22 and these changes are also replicated in patients with COVID-19 due to the severity of the disease, disease alone or due to the characteristic of viral pathophysiology, which is still poorly understood.23
Our study used the Perme Score as an instrument to assess patient mobility during their stay in the inpatient units. The Perme Score is a scale developed to evaluate patient mobility in the intensive care setting, taking into account conditions extrinsic to the patient who interfere with their mobility in the bed, such as the presence of supplemental oxygen device, endotracheal tube, many types of intravenous and intraarterial access and catheters, gastrostomy, nasogastric tube, chest drains, which can be interpreted as a barrier to mobility.11,12 Until then, no functional assessment instrument had taken these factors into account. Although evaluated outside the intensive care setting, our patients met the inclusion characteristics of the patients for the use of the Perme Score since they could have intravenous or intraarterial access, gastrostomy, nasogastric tube and chest drains and noninvasive ventilation. These data were described in 52.9% of the patients included in our study.
Pereira et al. also used the Perme Score to assess the functionality of patients undergoing liver transplantation at the time of hospital discharge, i.e., outside the intensive care setting. In this study, the average Perme Score at admission to inpatient units was 28 and at discharge 31. This score is close but not reaching the Perme ceiling, which is 32 points.24 When compared to the study by Pereira, our patients had lower mobility because the Perme Score at admission to IU was 17 points, with a significant gain of 7 points (p <0.001) until the time of hospital discharge, guiding the importance of the rehabilitation process still in the in-hospital phase but also making clear the impact of COVID-19 on the loss of mobility of patients.
Finally, with respect to the floor and ceiling effect of the instruments, a floor and ceiling effect of up to 15% is considered acceptable.25 One of the limitations of using Perme is the floor effect: patients who score zero on the scale due to sedation due to clinical severity, common for critically ill patients; and ceiling effect: patients who score 32 on the scale for not having any mobility deficit or barrier to mobilization, very common in patients in inpatient units. For our patient profile, a ceiling effect would be expected, i.e., that the patients had maximum values of the Perme Score. In the evaluation of the entry Perme Score, only 1 (1.4%) patient had a maximum score of 32 points.
Our results, added to the results published by Pereira et al., reinforce the applicability of its use in inpatient units and encourage future studies to validate the Perme Score in this new scenario.
In the intensive care environment, studies demonstrate that early mobilization reduces the length of stay in the ICU and length of hospital stay, reduces the number of days on mechanical ventilation and prevents physical deconditioning.26–28 It is worth mentioning that the gains are not only motor and how much the removal of the patient from the bed influences the improvement of pulmonary ventilation, improves oxygenation, and consequently reduces the need for ventilatory support in general.29,30 In recent decades, we have had significant gains in terms of mobility in the ICU.28,31 However, little is known about how well these gains are maintained in the transition from ICU to inpatient units and how long it takes to regain the mobility levels they had before admission.
Undoubtedly, using a single instrument to assess the patient’s mobility throughout their hospitalization journey would make more sense for the continuity of care in all phases of the rehabilitation process.
There are several instruments that assess the functional status in the ICU,9,10,32 but none that are used during the entire period of hospitalization. The hospital environment offers challenges to the rehabilitation process because, in addition to motor changes inherent to the individual, there is a range of devices used that offer restrictions to them and that should be considered during the therapeutic program appropriate to the patient’s condition.
For most patients, discharge from the ICU means an improvement in the patient’s condition and the beginning of a return to baseline functionality. However, an initial lapse in mobility activity may indicate the existence of barriers that prevent patients from promptly continuing their mobility trajectory from their achievements in the ICU. In the only previous study focusing on mobility activity in IU, Hopkins and colleagues32 found a decrease in activity within the first 24 hours in IUs.
The performance of motor physical therapy in the recovery of patients with COVID-19 has an essential role in gaining mobility, restoring physical independence, and recovering functional capacity.33,34 The prevention of the negative effects of immobility is a priority in preventing the loss of functional status of patients who develop severe conditions associated with COVID-19. Improving patient mobility, as evidenced by the Perme Score, decreases the length of hospital stay.26–28 Thus, therapeutic planning may include behaviour that prioritizes patient mobility through postural changes, sitting, standing, and walking when possible.35
Our rehabilitation program has been following the recommendation of the literature that proposes mobilization protocols based on the Perme Score, which certainly favours its implementation in practice, associating the assessment instrument with activity levels.15,36 It is divided into 5 phases and is performed depending on the clinical conditions of the patient, ranging from passive mobilization (phase 1) to independent gait (phase 5). Our results demonstrate that the mobility gain evidenced by the Perme Score was accompanied by advancement in the phases of the rehabilitation process. There was a transition of 39% of patients from phases 1 to 3 to phases 4 and 5 during the IU stay.
Limitations
Our study has limitations. The first is that the data were retrieved using a database, which limited our access to the patient’s previous health condition and possible comorbidities and limited the interpretation of the value of the Perme Score in its entirety. It would help if we had the data for all domains. The second is the heterogeneity of the sample in terms of sex (79.1% male), which may have influenced the results of comparing the Perme Score in terms of sex. The third is our small sample size. The fourth is the use of a non-validated instrument, as is the case with the Perme Score in inpatient units; however, one of the objectives of the study is to demonstrate the effectiveness of the instrument in the inpatient units to stimulate a validation study that will probably take place with our group.
Conclusion
The Perme Score proved effective for assessing mobility in patients diagnosed with COVID-19 with prolonged hospitalization outside the intensive care setting. In addition, we demonstrated by the value of the Perme Score that the level of mobility increases significantly from the time of admission to inpatient units until hospital discharge. The continuity of the assessment of the mobility level outside the intensive care environment provides the guarantee of evolution in the rehabilitation process. Thus, using the same instrument provides the comparison and measurement of the patient’s evolution throughout the entire period of hospitalization.
Acknowledgments
We thank the statistics team, especially for the help of Sandra Regina Malagutti.
Contributors
MSN made substantial contributions to study conception and design, data acquisition, analysis and interpretation of the data and has been involved in drafting the manuscript and revising it critically for important intellectual content; CT, RACE, SB, LLSG and FMS made substantial contributions to study conception and design and acquisition, analysis, and interpretation of the data and has been involved in drafting the manuscript and revising it critically for important intellectual content; FBT made substantial contributions to study conception and design and analysis and interpretation of the data and have been involved in drafting the manuscript and providing final approval of the version to be published.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing interest
All the authors declare no competing interests.
Ethics approval
This study was submitted to and approved by the Ethics and Research committee of the Hospital Israelita Albert Einstein, CAAE 5743322.2.0000.0071, and the Free and Informed Consent form was granted exemption. This study is in accordance with the recently amended Declaration of Helsinki of 1975.


_and_mean_(continuous_line)_in_the_perme_score_variation_between_.tiff)

_and_mean_(continuous_line)_in_the_perme_score_variation_between_.tiff)
