INTRODUCTION
The severe acute respiratory syndrome Coronavirus 2 (SARS-CoV-2) infection ranges from asymptomatic to pneumonia with acute respiratory distress syndrome (ARDS).1 The severity of the clinical presentation depends on host susceptibility, age, comorbidities, infectious strain, and viral load. Infection results in the production of high levels of inflammatory cytokines such as IFN-γ, IL-IL-6 and chemokines such as CXCL9.2
The primary need of patients infected with COVID-19 who come to healthcare facilities will vary depending on the case severity. In moderate to severe cases, they may require oxygen or ventilatory support. However, there can be limits to the availability of mechanical ventilation resources; therefore, efforts have been focused on finding alternatives, mainly in low-income countries.3 Patients requiring hospitalization are characterized by moderate to severe hypoxemia with high oxygen requirements. Due to the high mortality in patients who did not receive mechanical ventilation due to resource limitations,4 noninvasive ventilation (NIV) has been utilized as an alternative respiratory support strategy in managing patients with respiratory failure.5
Different types of noninvasive devices are used to treat ARDS related to COVID-19. These include high-flow nasal cannula,6 the helmet,7 the Wayrachi nasal continuous positive airway pressure device (NCPAP),8 and the modified snorkel mask.9,10 These devices are used in patients with ARDS who failed to improve with conventional oxygen therapy methods such as the venturi system or the reservoir mask and could not be admitted to the Intensive Care Unit (ICU) due to bed availability.11
The snorkel mask was initially modified by Ferrone in Italy for NCPAP delivery.12 In our hospital, a second modification was made to the mask, adding positive end-expiratory pressure (PEEP) pressure valves, decreasing the length of the corrugated tubing to reduce dead spaces, and adding a double oxygen intake system through a venturi device and another reservoir system.13 Throughout the COVID-19 pandemic at the Daniel Alcides Carrion Hospital, Huancayo-Perú, the modified snorkel mask has been the most widely used device for NIV support, even though other systems were available. In this hospital, there was an entire intermediate care unit for the use of NIV devices with the snorkel mask.14,15
This study aimed to analyze the effect of using a snorkel mask as a NIV system in patients with ARDS admitted with COVID-19.
METHODS
Ethical approval
The study protocol was approved by the Medical Research Ethics Committee of Daniel Alcides Carrion Hospital, Huancayo, Perú (approval No. 16-2021-CEI-HDAC). The study team is committed to protecting patient privacy and complying with the Helsinki Declaration.
Population
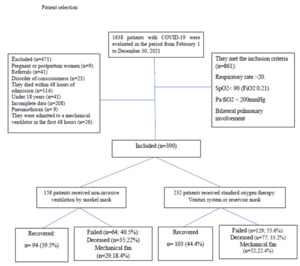
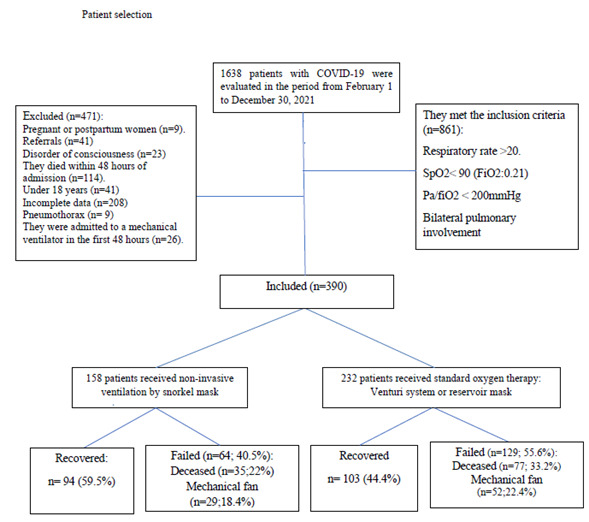
Eligible patients for this study were those diagnosed with COVID-19 via SARS-CoV-2 reverse transcriptase polymerase chain reaction or rapid antigen testing. The inclusion criteria were: (1) age > 18 years; and (2) bilateral lung injury or moderate/severe disease. The diagnosis of moderate disease included those with respiratory symptoms and bilateral lung lesions confirmed on chest imaging. Severe disease included those with at least one of the following two conditions: (1) SpO2 ≤ 90 % while breathing ambient air, or (2) PaO2/FiO2 ≤ 200 mmHg.16 Exclusion criteria included: (1) patients with impaired consciousness, (2) patients with pneumothorax, (3) patients using accessory muscles, (4) patients transferred to another health facility, (5) patients who died within 24 hours of hospitalization to minimize time bias,14 and (6) patients who were admitted to a mechanical ventilator within the first 48 hours of admission (Figure 1).
The ROX index was used to predict the success of oxygen therapy through the snorkel mask, which combines oxygenation (SpO2/FiO2) and the work of breathing (FR)= [SpO2/FiO2]/FR). The index was also used to assess the risk of failure of the snorkel system (i.e., admission to mechanical ventilation or death). Cases included patients receiving oxygen by snorkel mask plus standard therapy, and controls receiving oxygen by Venturi mask or variable FiO2 reservoir bag plus standard therapy.
Study Design
We analyzed the data of 1,638 patients hospitalized for COVID-19 from February 1 to December 30, 2021 (the date of admission of the last enrolled patient) at the Daniel Alcides Carrion Hospital in Huancayo, Perú. The data set includes comprehensive clinical information on diagnoses, treatments, oxygen requirements, complications, ICU admissions, imaging, laboratory results, discharge, or death.
In this retrospective case-control study, the outcome of interest was the frequency of improvement of enrolled patients, defined as discharge with recovery. Snorkel failure was defined as the initiation of mechanical ventilation or death. Secondary endpoints were the rate of recovery from hypoxia, ROX index, and length of hospital stay. Hypoxia was defined as oxygen saturation below 90% when inhaling ambient air, according to the values at altitude (3200 meters above sea level). The worsening of hypoxia is defined as an increased requirement of oxygen concentration to maintain normal oxygen saturation resulting in the utilization of mechanical ventilation or death.17
The decision to intubate a patient was left to the treating physician’s discretion. However, it was generally based on the following criteria: failure to maintain SpO2 > 88% despite receiving the maximum allowed FIO2, persistence or worsening of respiratory failure (PaO2/FiO2<100 mmHg, respiratory rate > 35/min) with associated respiratory distress, development of conditions requiring endotracheal intubation to protect the airway (e.g., coma or seizure disorder), severe metabolic acidosis, or to manage copious bronchial secretions. The patients also received complementary therapies according to the COVID-19 management guide and as indicated by the treating physician. This therapy commonly included systemic glucocorticoids, paracetamol, pronation, cough suppressants, and the infrequent use of convalescent plasma.
The authors extracted data in a structured format, including clinical data before applying the snorkel mask, during the procedure, and 4 hours afterward. The ROX index was recorded before, 4 hours after applying the snorkel mask, and at the patient’s discharge. Laboratory data were collected in the same way.
About the Noninvasive Ventilation System with Modified Snorkel
The snorkel system consisted of a snorkel diving mask that presents a complete separation between the inspiratory and expiratory circuits. An internal silicone pocket covers the mouth and nose where fresh oxygen enters through non-return valves. The exit of exhaled CO2 is through four valves. One is located on each side of the nose. The other two are channelled into the internal side tubes through a pair of non-return valves connected to a piece of polycarbonate known as the Charlotte valve. This valve contains a triple mouth, the first connected to the mask, the second to the exhaled air outlet, which was connected at the end to an adjustable cylindrical valve of PEEP and then to a ventilatory filter to prevent air contamination with viral particles. The third was the air intake channel, which was connected to a humidifying filter and later to a double independent oxygen intake flow consisting of a venturi system and another to the reservoir mask, each with an independent oxygen point, and each one was independently connected to 15 litres of oxygen per minute, which was to be reduced according to the patient’s response (Figure 2).
Installing the snorkel device consisted of placing the patient supine, hermetically fixing the mask on the patient’s face to avoid air leaks, setting the valve with PEEP at zero, and administering 15 litres of oxygen. Once oxygen saturation improved, the patient was placed in a prone position. After ten minutes, the alveolar recruitment maneuvers were started, consisting of the progressive increase in PEEP in the following order: zero to 2.5 cm H2O, then 5 cm H2O and finally to 10 cm H2O, each change after ten minutes. The patient remained in this position for at least four hours, followed by a 2-hour rest period with a reservoir mask (15 litres/min). After that, weaning from snorkelling was done according to clinical improvement.
Statistical analysis
All statistical analyses were performed using the statistical program STATA v.14.0. The Chi-square test or Fisher’s exact test was used to compare the control and snorkel groups. The continuous variables were presented with mean, interquartile range and standard deviation. A comparison of these was then performed with the Mann-Whitney U test. All statistical tests were bilateral, considering p<0.05 as statistically significant. Cox regression modelling was used to determine the probability of failure of snorkel treatment. Hazard ratio (HR) values derived from structural models were adjusted for age and gender.
Sample
Due to limited knowledge of the snorkel mask efficacy, we assumed a resolution rate for the snorkel group of 30% and a resolution rate of 13% for the control group based on a first pilot study of 30 patients for each cluster. We estimated that 144 participants were required for the snorkel group. The sample size increased by about 10% due to incomplete data. Therefore, the trial was designed to include 158 snorkel mask wearers. Enrollment was carried out in a non-randomized consecutive manner until the sample size was reached. The patients who did not use the snorkel mask and met the inclusion criteria were considered part of the control group.
RESULTS
Out of 390 patients who entered the study, 158 used the snorkel mask, and 232 received standard-of-care treatment according to the management guidelines of the institution. The population’s average age was 54, and 70% of all patients were male. Of the comorbidities identified, diffuse interstitial lung disease was identified in 32% of participants. Chronic diseases such as diabetes mellitus and arterial hypertension were found in 24% and 11% of the patients. No significant differences were found in the baseline characteristics of both groups (Table 1).
The total average body mass index was 28.5 kg/m2. The mean length of illness at the time of hospital admission was nine days. The average respiratory rate was 25 per minute; oxygen saturation on admission averaged 78.7%, and the mean ratio of arterial oxygen pressure to the fraction of inspired oxygen (PaO2/FiO2) was 138. The average lung involvement of patients with COVID-19 evaluated by tomography was 57%. Ground glass opacities were present in 56.6% of patients, and diffuse consolidation was evident in 38%.
With snorkel mask treatment, 57% of all patients improved. In the group that received standard therapy, it was 44.4% (P=0.046). Patients who required a mechanical ventilator comprised 20.7% of the total population, 22.4% in the group that received standard treatment and 18.4% in the group that received snorkel masks P<0.001). The mean number of days of snorkel masking was six (Table 1).
The total number of deaths was 28.6% of the study population. The percentage of deaths in the group that received the snorkel mask was 22%, and in the standard therapy group was 33% (P=0.023). The rate of recovery was 59.5% in patients in the snorkel mask group and 44.4% in the group that received standard treatment (P=0.046).
The most frequent complications during hospitalization were nosocomial pneumonia (17.8%) and pulmonary thromboembolism (4.26%). Overall hospital stay was 12.9 days on average, 17.2 days in the snorkel group, and 10.6 days in the standard therapy group.
Comparing the respiratory parameters in the patients who received the snorkel mask, the average values were separated before using the device, 4 hours after the use, and at hospital discharge. The average PaO2/Fio2 remained similar before and 4 hours after using the NIV snorkel, while at discharge, these values were 240 on average. The pre-snorkel ROX index was 4.57, and 4 hours later, it was 4.99, while at discharge, the average of this index was 19.45 (Table 2).
Factors associated with snorkel device failures were: (1) consolidation-type tomographic pattern compared to the other patterns (HR 1.56; 95% CI 1.02-2.35: P=0.036), (2) presenting some complication such as nosocomial pneumonia or thromboembolism (HR 1.22; 95% CI 1.05-2.35: P=0.008) and (3) a pre-snorkel ROX index < 4.8 (HR 1.2024; 95%CI 1.024-2.41: P=0.037) were associated with failure to use NIV-snorkel (Table 3).
The comparison of the risk curves showed the lowest probability of dying or requiring a mechanical ventilator in the group of patients who used the noninvasive system with snorkel (log-rank test P-<0.001) (Figure 3). No clinical improvement to the use of the snorkel mask occurred in 74/158 (46.8%) patients, and in the group that did not use the snorkel mask, 129/232 (55.6%) patients failed.
DISCUSSION
In this study, 390 patients were hospitalized for respiratory failure related to COVID-19 infection. A significant number were successfully managed with the modified snorkel mask and did not require mechanical ventilation, reducing overall mortality by 11% (P=0.023). These data suggest that snorkel mask use during COVID-19 has the potential to decrease the need for invasive mechanical ventilation. We also observed an increase in hospital stay by seven days in the group that received NIV with the snorkel, compared to the group that received standard treatment.
A study comparing the snorkel mask with other systems demonstrated better ventilator-patient interaction in terms of shorter pressurization time and shorter expiratory time delay, better interface performance underscored by lower trigger pressure drop (ΔPtrigger), and higher pressure-time product, which can be explained by the reduced internal volumes of the snorkel mask.12 Likewise, it showed stability in maintaining the PEEP level at 10 cm H2O. Based on this result, the hospital use protocol aimed to maintain PEEP at 10 cm H2O to meet the alveolar recruitment objective. The other parameters compared in terms of maximum inspiratory deflection (ΔPawi) and peak inspiratory (ΔPawe) did not show significant differences.9,12 Another study incorporated an enteral feeding route into the snorkel mask to avoid interruption of respiratory care with good results, unlike our study, where the patient had to remove the snorkel mask to receive food.18
Avoiding the mechanical ventilator may allow a reduction in complications commonly associated with endotracheal intubation, such as pneumonia, ventilator-associated lung injury, or secondary infections. In addition, avoiding intubation by using a snorkel can help conserve ventilators in the event of a shortage. However, despite these advantages, there is concern that the poor selection of patients with pathologies that affect the ventilatory mechanism (e.g., neurological disorders, respiratory muscle fatigue) could lead to NIV failure. Its functionality depends on the respiratory strength of the affected person.19
It has been suggested that given the prolonged duration of COVID-19 illness, adequate use of NIV may have a low failure rate and may delay endotracheal intubation.20 This study provides evidence that snorkel mask use in patients with COVID-19-related respiratory failure is associated with favourable clinical outcomes. In addition, a decrease in hospital mortality and utilization of a mechanical ventilator was demonstrated. Despite these findings, we accept that the decision on the timing of intubation is specific to each patient. Poor selection of patients for mask use is also likely to lead to unfavourable clinical outcomes; however, early evaluation within four hours of initiating snorkel use may indicate failure and prompt an immediate search for a mechanical ventilator.
The results suggest that the ROX index will help select the patients who are likely to be successful with this NIV device and avoid initiating mechanical ventilation. This index has also been used as a predictive indicator in other noninvasive systems, such as the use of high-flow cannula.21,22 This index was also used to predict success after four hours of use, so it is important to monitor this parameter early to identify the success of the snorkel mask.
Our results indicate that in respiratory failure related to COVID-19, the snorkel device can be used before endotracheal intubation. The variation in the ROX index can be evaluated four hours later to assess the need for mechanical ventilation, similar to the use of other non-respiratory devices.23 In the multivariate analysis, a ROX index <4.8 was significantly associated with failure to use the snorkel device.
The disadvantage of using the snorkel mask is the high oxygen consumption, which can cause drops in hospital oxygen pressure. Likewise, this device requires the doctor to remain next to the patient, mainly during the first hour of use, to progressively increase the PEEP values until reaching 10 cm H2O in the supine position. This avoids air leaks that favour a drop in inspiratory pressures and the appearance of asynchrony. In the post-COVID pandemic era, where a high number of mechanical ventilators are available, the use of a snorkel mask may be a therapeutic alternative for patients with moderate or severe atypical pneumonia with high oxygen requirements before opting for the use of the mechanical ventilator and through its use try to reduce the complications generated by invasive ventilation.24 It seems to be a better alternative than the other NIV systems.25
This study has some limitations. First, this was a retrospective observational study. Although attempts were made to correct for covariates, all confounding factors, such as any additional treatments, may not have been accounted for. Second, our study may not have been able to detect differences in clinical and laboratory outcomes between groups. However, given the results, the snorkel device is highly suitable for application in clinical care, given its ability to reduce the need for mechanical ventilation. Prospective trials are required to explore these advantages further.
CONCLUSIONS
The modified snorkel mask can be used as an acceptable alternative to other forms of NIV and as an early-use alternative before considering the utilization of a mechanical ventilator. The use of a snorkel mask reduced mortality in patients with ARDS due to COVID-19.
Acknowledgments lack
To Dr. Patrick Elliott for the final review of the manuscript.
Contributors
All authors contributed to the conception or design of the work, the acquisition, analysis, or interpretation of the data. All authors were involved in drafting and commenting on the paper and have approved the final version.
Funding
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing interests
All authors have completed the ICMJE uniform disclosure form and declare no conflict of interest.
Ethical approval
The study was approved by the Medical Research Ethics Committee of Daniel Alcides Carrion Hospital, Huancayo, Perú (approval No. 16-2021-CEI-HDAC).


_of_patients_with_coronavir.jpeg)

_of_patients_with_coronavir.jpeg)