Introduction
Respiratory distress syndrome (RDS) is one of the major morbidities in Neonatal Intensive Care Units (NICU). Premature neonates develop RDS due to their limited ability to produce endogenous surfactant.1,2 Surfactant replacement therapy is one of the standard treatments for RDS. Traditionally, the Intubation, Surfactant Administration and Extubation (In-Su-RE) method has been used to facilitate intra-tracheal surfactant delivery and has been shown to reduce the need for mechanical ventilation.3,4 However, over the last decade, surfactant administration via thin catheters in spontaneously breathing neonates has become increasingly popular as it precludes the need for endotracheal intubation and positive pressure ventilation. This method is often referred to as Minimally Invasive Surfactant Administration (MIST) or Less Invasive Surfactant Administration (LISA).5–7
A growing body of literature has demonstrated MIST/LISA to be feasible and safe in premature neonates.7,8 A recent network meta-analysis comparing In-Su-RE and MIST/LISA demonstrated that the latter technique was associated with a significantly lower mortality rate, need for mechanical ventilation, bronchopulmonary dysplasia, and periventricular leukomalacia.9 Although MIST is widely accepted as a primary mode of surfactant administration in some neonatal centers, considerable variation exists regarding procedural aspects. These include the choice of premedication, catheter choice, and post-procedural support.10,11
Studies report the use of widely varying types of catheters (e.g., nasogastric catheters, suction catheters, and vascular catheters) for MIST.12 In Europe, purpose-built catheters for MIST have been used in the last 5 years.12 In Canada, purpose-built catheters have only recently received approval for use. However, limited data are available on the use of these types of catheters. More data regarding procedural success, adverse effects, and end-user experience with these purpose-built catheters are needed to optimize clinical practice and direct future product design and development. Therefore, we designed this study to describe the local experience with two different purpose-built catheters (BLEScath™ and SurfCath™) for MIST.
Methods
This was a retrospective cohort study of neonates who received surfactant via MIST using any of the two purpose-built catheters (BLEScath™ and SurfCath™) approved for use in a tertiary-level NICU in Southwestern Ontario. The institutional ethics board approved the study (HSREB no.119981). The aim of this study was to describe procedural success, adverse events, and user experience pertaining to the two different types of purpose build catheters for surfactant administration.
Study Eligibility Criteria
All neonates who received MIST by a purpose-built catheter from January 1, 2021, to March 31, 2022, were included (see Table 1). We excluded neonates who received surfactant by IN-Su-RE method, received surfactant by MIST using non-purpose-built catheters [angiocath, multiaccess catheter (MAC)] and neonates suspected to have chromosomal or congenital anomalies.
MIST procedure Details
In our institute, MIST procedure was recommended as the first option for surfactant administration in spontaneously breathing neonates with a gestational age of ≥ 26 weeks gestation and RDS (FiO2 >/=0.30 on non-invasive positive pressure ventilatory (NIPPV) support with a Mean Airway Pressure (MAP) of ≥ 8 cm H20). Neonates with poor respiratory drive (defined as >3 apneic episodes in the hour preceding surfactant delivery), hemodynamic instability (hypotension), birth asphyxia, and major congenital anomalies were not considered suitable candidates for MIST. Premedication with fentanyl 0.5 mcg/kg intravenous (IV) and Atropine 20 mcg/kg IV was recommended, and the use of oral sucrose was encouraged.
Trained physicians (subspecialty residents/staff neonatologists) and respiratory therapists (RT) performed the procedure. Neonates were positioned in a sniffing position and received nasal intermittent positive pressure ventilation (NIPPV) using nasal prongs for the entire procedure.
The depth of catheter insertion was 6 cm + weight in kilogram (kg) as measured from the lip. Cords were visualized either using direct laryngoscopy or through video laryngoscope. Bovine Lipid Extract Surfactant (BLES®) at 5 ml/kg was administered slowly over 1 to 3 minutes, synchronizing instillation with the neonate’s inspiration efforts. After successful catheter placement, the laryngoscope and catheter were withdrawn, and attempts were made to keep the neonate’s mouth closed to facilitate continued delivery of positive airway pressure. Post-procedure, stomach contents were aspirated via a nasogastric/orogastric tube to check for accidental instillation in the esophagus and to assess for substantial pharyngeal reflux. As per the institutional protocol, there were a maximum of three attempts. Attempts were defined as any introduction of a laryngoscope blade followed by removal regardless of the successful catheter placement. Failed attempts refer to failure to place intratracheal catheter or displacement of the placed catheter without completing surfactant delivery.
MIST Catheter Description
Since introducing MIST to our NICU in 2016, the local quality improvement committee has monitored its safe and effective implementation. Under the committee’s guidance, commercially available purpose-built catheters (BLEScath™ and SurfCath™) were assessed in the NICU using predesigned forms that collected procedural data and user ease. Then, the catheters were introduced one by one in specific and equivalent periods.
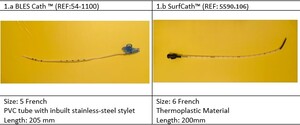
BLEScath™ is 205 mm long, 5 FR with integrated stainless steel (SS) stylet that is anchored and remains fixed in place, with 7-10 cm marking on the catheter to determine tip-to-lip distance. Manufacturers state that the SS stylet allows the catheter to be bent into the user’s preferred shape. Additional distal tip markings (2/2.5/3.5 cm) aid in determining the catheter insertion depth at the vocal cords. The tip of the catheter is soft and rounded to reduce tissue trauma during insertion (Figure 1a).13
SurfCath™ is a 20 cm, 6 FR tube made of a thermoplastic material anatomically designed with a 2 cm black tip at a 30-degree angle. The catheter is transparent, with clear markings for each centimetre, and the material is semi-rigid but bendable (Figure 1b). In addition, it has an extra soft tip to reduce damage to the vocal cords.14
Data Collection
Baseline demographic characteristics were collected from patient charts, including gestational age, weight, antenatal steroids, maternal chorioamnionitis, mode of delivery, resuscitation details and respiratory support prior to the procedure. Data regarding the procedure were extracted from the completed procedural forms. They included the type of catheter, type of operator, premeditations used, number of attempts, successful delivery of surfactant, oxygen requirement post surfactant, the subsequent need for mechanical ventilation and/or the need for a second dose of surfactant.
Data were also collected regarding complications, including apneas, desaturations (oxygen saturation < 85%), bradycardia (heart rate <100 beats/min), need to use Positive Pressure Ventilation (PPV)/need to intubate during the procedure, and air-leak. Our primary outcome of interest was procedural success, defined as intratracheal delivery of the full intended dose of surfactant with minimal to no surfactant recovered on post-procedure gastric aspiration. Our secondary outcomes included a number of attempts to achieve procedural success and procedural ease of use, where users rate their experience as very easy, relatively easy, neither easy nor difficult, somewhat difficult or very difficult.
Statistical Analysis
Continuous variables were summarized using means (SDs), and group comparisons were conducted using independent t-tests. Categorical variables were summarized using frequencies (%), and group comparisons were conducted using chi-square tests (or Fisher’s exact chi-square, when appropriate). P-values < 0.05 were considered statistically significant, and SPSS v.26 (IBM Corp., Armonk, NY, USA) was used to conduct all analyses.
Results
A total of 37 neonates received MIST during the study period. BLEScath™ was used in 15 neonates, and SurfCath™ was used in 22 neonates. Baseline patient characteristics are described in Table 1. The type of operators differed in the two groups, with a higher proportion of RT operators in the SurfCath™ group.
Procedure success rate, ease of use and adverse effects are summarized in Table 2. The procedural success was 93% in the BLEScath™ group and 91% in the SurfCath™ group (P >0.994). Multiple attempts to successfully administer the surfactant were required in 33% of BLEScath™ and 23% of SurfCath™ (P=0.708). Response to surfactant was noticed in 75% of the BLEScath™ group compared to 91% of the SurfCath™ Group (P=0.300). 90% of neonates in the SurfCath™ group were weaned to room air within 24 hours compared to 63% in the BLEScath™ group (P=0.123).
Desaturation was the most frequently observed adverse event during the procedure; it was reported in 60% of the BLEScath™ group and 77% of the SurfCath™ Group (P=0.29). The next frequent adverse event was apnea, which occurred in 60% of the BLEScath™ group and 46% of the SurfCath™ group. For post-procedural complications, air leak occurred in two neonates in the BLEScath™ group and three in the SurfCath™ group (P>0.994).
On analyzing user experience, 52% of operators using SurfCath™ felt it was “very easy” to use compared to only 14% of operators of BLEScath™. Thirty-three percent of BLEScath™ users felt it to be “somewhat difficult” and “very difficult,” whereas only 5% of SurfCath™ users reported difficulty (P=0.021).
Discussion
Our center has practiced MIST since 2016 and remains one of the most experienced units with this technique in Canada. Different catheters for surfactant delivery have been used locally over the last six years. We have previously reported our earlier experience with off-label catheters such as 16G Angiocath and Multiaccess Catheters (MAC).5 Purpose-built catheters have recently been approved for use in Canada and introduced in our unit under careful evaluation for safety and efficacy by the local quality improvement committee, which allowed us to describe our experience with these catheters in this retrospective study. We report high procedural success with both catheters without any significant differences in procedural execution or procedural adverse effects. Subjective assessment of operator ease of use appears to be higher with SurfCath™ compared to BLEScath™. Overall procedural success with the purpose-built catheters appears to be comparable to our previous experience with non-purpose-built catheters in which we reported a success rate of around 90%,5 which is slightly higher than other studies using non-purpose-built catheters in which the overall success rate ranges from 73-89%.15–19
There is considerable variation in the choice of catheter for MIST. A recent survey of MIST use in Canada reported that 47% of centers using MIST utilize Angiocatheter to deliver surfactant, whereas 41% use purpose-built catheters.20 Some centers still report the use of feeding tubes. Among the centers that do not use MIST, 22% cited the lack of availability of purpose-built catheters as the reason for the non-implementation of MIST. A US survey published in 2019 reported that 46% of physicians used feeding tubes for surfactant administration, 20% used angiocatheters (Hobart method), 4% used umbilical catheters, and 30% used other methods that were not specified.
Purpose-built catheters offer many advantages over traditionally used catheters and will undoubtedly increase institutional uptake and adaptation of MIST. The advantages of purpose-built catheters include markings/graduations to guide depth of insertion, rigidity to facilitate negotiating through cords without using Magill’s forceps, atraumatic design to protect the airway, and curvature to adapt to neonatal airway anatomy. BLEScath™ has an inbuilt stylet designed to add rigidity to a pliable tube. Manufacturers describe SurfCath™ as semi-rigid but bendable.13,14 Despite the differences in design, the overall success rate was similar with both catheters.
The number of failed attempts in the BLEScath™ group was higher than in the SurfCath™ group (33% vs 23%), but this difference was not statistically significant. Immediate response to surfactant was noticed more in the SurfCath™ group. A higher number of neonates were weaned to room air by 24 hours in the SurfCath™ group, but these differences were not statistically significant. The subjective reporting of ease of use favoured SurfCath™, with more operators reporting improved ease of use with SurfCath™. On qualitative assessments of procedural forms, we noted user comments related to the too-pliable nature of BLEScath™ as a recurring theme that interfered with operators’ perceived ease of use.
Interestingly, Rigo et al. investigated different devices used for LISA and found that more rigid catheters, such as the Angiocath, permitted faster laryngeal catheterization than gastric tubes. In the same study, the subjective ease of use of rigid catheters was also reported to be better.21 In 2018, Fabbri et al. described the clinical impressions of neonatologists who simulated LISA on an extremely premature manikin to compare the new purpose-built LISAcath and the commonly used Angiocath. Results of this study showed that the neonatologists preferred LISAcath rather than Angiocath and perceived it to be the safer option.22 While the rigidity of a catheter may offer procedural benefits, a balance between pliability and rigidity should be considered to avoid accidental airway injury. We have reported a case of airway injury and pneumomediastinum after MIST with semi-rigid 16G Angiocatheter.23
Regarding adverse events during the procedure, we noticed that desaturation was the most frequently reported event, followed by apnea. Interestingly, most of these events spontaneously improved with gentle stimulation. We only reported one case that required positive pressure ventilation during the procedure, and none required intubation during the procedure. The rate of air leak (pneumothorax and pneumomediastinum) in this cohort ranged from 13% in BLEScath™ vs 14% in SurfCath™ without any significant difference between the two groups. Pneumothorax rates alone are reported to be 5.5% with MIST methods and 9% with IN-Su-RE. While our rates of air leak are slightly higher, this may be because of including both pneumothorax and pneumomediastinum in the definition of air leak.24 In our cohort, the rate of needing intubation for any reason within one week of MIST was 20% in the BLEScath™ group and 30% in the SurfCath™ group without any significant difference. These rates are similar to that found in the literature, citing that the need for intubation for mechanical ventilation within 72 hours of the MIST procedure is around 22.8%, and the need for any mechanical ventilation during NICU stay is around 49%.24
We acknowledge that our study is limited by its retrospective design and small sample size. Our secondary outcome related to ease of use was subjective in nature and prone to bias. The distribution of operators was different in the two catheter groups with more RTs using the SurfCath™, which could potentially lead to confounding bias. Additionally, the catheters were introduced sequentially, not simultaneously; hence, cumulative operator experience could be a factor in the perceived ‘ease of use.’ Lastly, we did not address cost and other financial implications.
Conclusion
This is the first study in Canada to report the experience of MIST with purpose-built catheters. Overall, the success rate was equally high in both catheters. Users subjectively reported higher ease of use with SurfCath™ compared to BLEScath™. Commercially available purpose-built catheters should facilitate universal adaptation of the MIST method. Our reports regarding operator experience may help optimize future product design to improve ease of use.
Acknowledgments
We would like to acknowledge the help of Dr. Natasha Lepore for assisting with the data collection for this project. We extend our gratitude to the Division of Neonatal-Perinatal Medicine and the healthcare team.
Contributors
TA was involved in data collection and manuscript preparation. MM was involved in data analysis and interpretation. ODS helped design the study and in manuscript preparation. SB was responsible for the conception of the study, study design, data collection, interpretation and manuscript preparation. All authors have approved the final version.
Funding
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing interests
All authors have completed the ICMJE uniform disclosure form; ODS received professional consulting fees from BLES Biochemical Inc. in the past. BLES Biochemical Inc. did not fund the study nor have any influence in the design, data collection, and interpretation of the results. The surfactant maker did not review or revise the manuscript submitted for publication. No catheter manufacturer had any influence in the study design, data collection and interpretation of the result. Other authors have no conflicts of interest to declare.
Ethical approval
The REB approved the study (HSREB no.119981).