Background
Respiratory therapists (RTs) are specialized healthcare professionals who provide essential care to individuals across the lifespan with acute and chronic cardiorespiratory conditions. The scope of respiratory therapy (RT) practice is broad, encompassing responsibilities such as performing and collecting diagnostic information, patient assessment, applying therapeutics to respiratory care (e.g., aerosol therapy, artificial airways), and disease management to discharge planning.1,2 RTs play vital roles in diverse settings, including intensive care units, operating rooms, neonatal and pediatric wards, rehabilitation clinics, and patients’ homes. Despite this breadth, RTs practice in an increasingly resource-constrained environment,3,4 where demonstrating impact, optimizing care, and contributing to system-wide efficiencies constitute a clinical imperative and professional responsibility.5
Given the need to justify professional contributions amidst rising system pressures, the practice of RT should be grounded in evidence.6–8 Advancing the evidence-informed practice of the RT profession will strengthen the credibility, visibility, and sustainability of the profession while improving patient outcomes. However, while research exists to support many aspects of RT practice,9–11 much of this work has been generated by other professions (e.g., physicians, nurses, physiotherapists), where research questions and agendas may not fully reflect the priorities or nuanced realities experienced by RTs. Consequently, certain dimensions of the RT profession and practice likely remain underexplored.12,13 This reliance on externally generated evidence contributes to a fragmented knowledge base that does not fully reflect the scope, complexity, or contextual realities of RT and may perpetuate gaps in care, professional autonomy, and role optimization.13,14
Establishing clear research priorities that reflect the professional experiences, expertise, and needs of RTs is important to inform funding and policy decisions, guide future research projects and align continuing professional development efforts. One common way to identify these shared priorities is through consensus-based research methodologies, which provide structured ways to synthesize expert perspectives where empirical evidence is limited.15–18 Among these, the Delphi method involves a structured, iterative process that engages diverse knowledge users across multiple rounds to build consensus and refine expert judgment.
Although Delphi methods are widely used in research across health disciplines19–21 and have been applied to respiratory-related topics,22,23 RTs are rarely included as knowledge users in these studies.24 Reviews of the literature indicate that RTs are often underrepresented (or absent) from expert panels, even in topic areas where they play a central clinical role.24 This exclusion risks producing research agendas that might not reflect the realities of RT practice and may overlook knowledge gaps that RTs themselves consider important. To address this gap, we conducted a pan-Canadian Delphi study to identify and prioritize research needs across the RT profession. This study builds on findings from a prior qualitative description study that explored the knowledge gaps and research needs reported by Canadian RTs.25 The objective of the current study was to seek consensus on the prioritization of research needs for the RT profession in Canada.
Methods
Study Design
We used a modified Delphi method to identify research priorities and knowledge gaps in the RT profession. A modified Delphi is a variant of the classic Delphi technique that integrates qualitative and quantitative methods.17 In this approach, participants are presented with a structured list of items generated from prior research.17 In our study, the items were informed by an earlier qualitative description study to identify what experts perceive as the knowledge gaps and research priorities.25 These findings informed the development of items for a national Delphi online consensus survey, which was administered in two subsequent rounds across Canada. When preparing this manuscript, we were guided by the Delphi studies in social and health sciences—Recommendations for an interdisciplinary standardized reporting (DELPHISTAR) checklist to support clear and comprehensive reporting.26 This study received research ethics board approval from the Hospital for Sick Children (SickKids, #1000079058) and Ontario Tech University (#16789).
Participant Eligibility Criteria and Sampling
Participants were eligible if they were registered RTs. Specifically, they had to be registered with their respective provincial regulatory body or with the Canadian Society of Respiratory Therapists (CSRT), be fluent in English or French (reading and writing), have access to internet, and have provided written informed consent. Student RTs were excluded because they could not provide informed perspective on the current knowledge gaps in practice.
We used a convenience sampling approach to recruit participants from the RT population in Canada (n = 12,291).27 To recruit the highest number of RTs, a multi-modal recruitment strategy was used, which included disseminating a link using the e-mail lists of the CSRT and the Ordre Professionnel des Inhalothérapeutes du Québec (OPIQ), to ensure recruitment efforts reached both anglophone and francophone RTs across Canada. Supplementary strategies included periodic “e-blasts” on CSRT’s social media platforms28 and encouragement to participants to forward the online survey link to other RTs not on the e-mail lists (i.e., snowball sampling).29
Participants were invited to complete any or all rounds of the Delphi survey. Recruitment remained open for both rounds, so each round included a mix of new respondents. Because the survey was anonymous, the exact proportion of participants who completed both rounds could not be determined. Informed consent was obtained online before completing the survey. To ensure diverse representation, we sought participation from RTs across seven key areas of practice: in-patient respiratory care, community and chronic care, cardiopulmonary diagnostics, anesthesia assistance, management/administration/leadership, neonatal/pediatric care and education in entry-to-practice respiratory therapy programs.25,30 There is no universally accepted standard for the expert panel sample size in Delphi studies; however, panels of 15 to 30 experts from the same discipline have been suggested.31–33 Regardless of the number, it is more important to focus on the quality of the participants to ensure representativeness in the panel.34
To minimize attrition across rounds of surveys, we implemented certain strategies. Participants were able to complete their survey in multiple sittings using a return code and were eligible to claim CSRT continuing education hours as compensation for their time.
Delphi Survey
The items for the online survey were based on four domains, as reported previously by Zaccagnini, et al.25 The lead authors (SQ, MZ) generated a preliminary list of items organized according to each of the four domains: 1) System-level impact of RTs; 2) Optimizing RT practices; 3) Scholarship on the RT profession; and 4) RT education. These items were iteratively reviewed and refined through multiple team meetings to ensure clarity and relevance.
Once the preliminary items were agreed upon, they were pilot tested in English by three RTs who each had more than five years of broad experience in the practice areas of RT. Specifically, we asked them to review each item and provide written feedback regarding the wording, clarity and relevance. After integrating their feedback, surveys were translated into French using a professional service (Transtao Global, Saint-Laurent, QC).
The surveys were mounted and administered using REDCap, a secure, web-based data capture platform hosted on servers licensed and maintained by the Hospital for Sick Children (SickKids, Toronto, ON). The research team conducted a usability check of the REDCap platform to ensure survey functionality and accessibility before disseminating the survey. The final survey for the first round (R1) included 74 items across the four domains (System-level impact of RT = 17; Optimizing RT practices = 19; Scholarship on the RT profession = 26, and RT Education = 12). Each domain also included an open-ended question inviting participants to suggest additional items that they believed are important to consider for subsequent survey rounds.
For subsequent survey rounds, the number of statements for each domain depended on the participants’ feedback and whether consensus was achieved. Items that reached consensus in any round were removed from future rounds to reduce response burden and minimize participant attrition. Survey revisions were made by the research team and included minor grammatical edits and/or content suggestions based on open-text feedback. To mitigate potential response bias due to survey fatigue, item order was randomized in subsequent rounds to discourage participants from only completing the initial sections. The English and French surveys are available in Supplementary File 1.
Data Collection
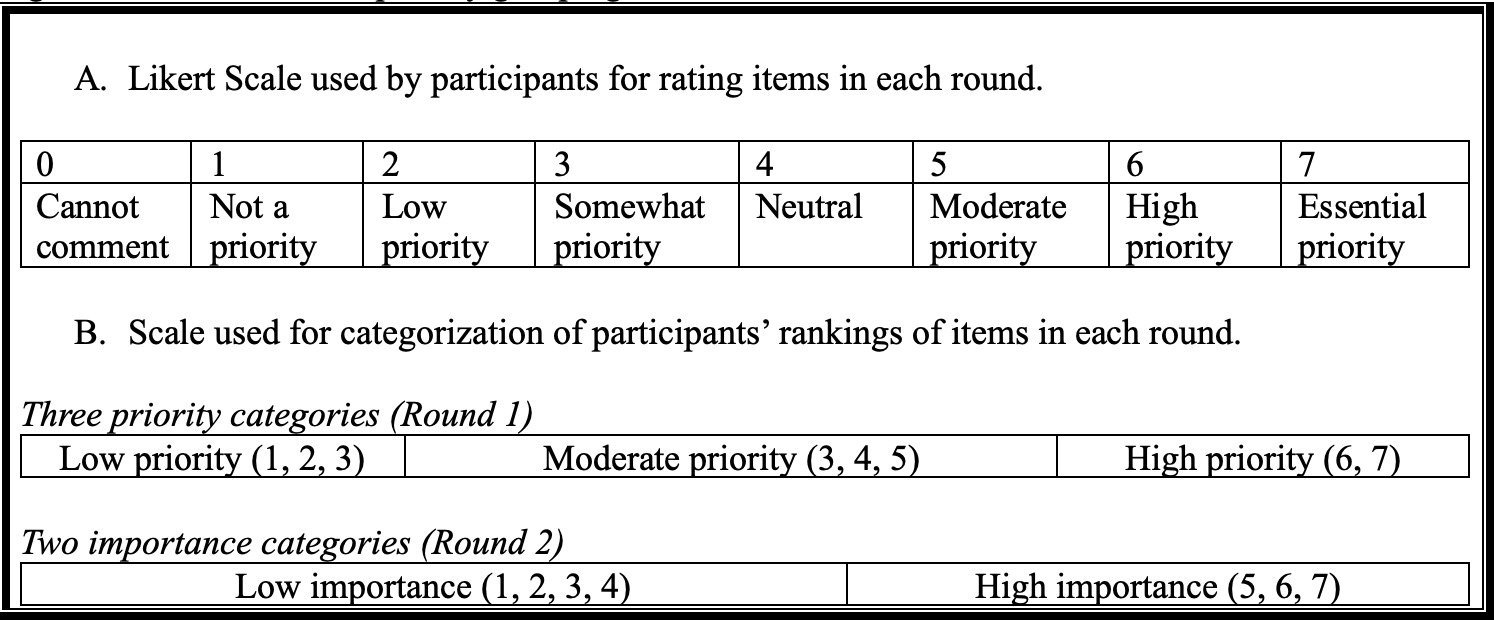
Baseline demographic characteristics were collected at each round as RTs may complete one or all rounds of the Delphi survey. For each statement across the domains, participants were asked to rank each item using a seven-point Likert scale ranging from “1=not a priority” to “7=essential priority,” shown in Figure 1. If a participant self-determined they were unable to assess the research priority due to limited knowledge in that area, they were able to select “0=unsure/cannot comment.” R1 was open for participation from January 1 to March 17, 2024, and the second survey (R2) from August 27 to December 31, 2024.
Data Analysis
Participant baseline characteristics were described using means, standard deviations (SD), medians, interquartile ranges (IQR), frequencies, and proportions depending on the data variable. Survey responses were excluded from analysis if participants completed less than 75% of the items in a given round. Survey responses from each round were analyzed using frequencies and proportions of Likert scale responses (Figure 1). Responses marked as “0 = unsure/cannot comment” were excluded from the consensus analysis for each item to avoid inflating agreement or disagreement. Subgroup analyses were conducted based on participants’ primary area of practice to explore variation in research priorities across clinical contexts.
Percentage-based agreement is the most widely used data analysis method in Delphi studies, with reported thresholds typically ranging from 50% to 100%, and 70% to 75% being the most frequently applied.16,35 In some cases, adjusting consensus criteria during analysis may be necessary to ensure the findings of Delphi studies are practical and useable.36 For this study, consensus thresholds were defined a priori before data collection and revisited during analysis to enhance the specificity of identified research priorities.
In R1, we used a three-level classification to group Likert scale responses: low priority (ratings 1–2), moderate priority (3–5), and high priority (6–7). A threshold of ≥70% agreement was used to define consensus. Items that met this threshold were labelled as priorities.
In R2, no additional items met the ≥70% agreement consensus threshold. As a result, and to identify items that might still be viewed as important even if not prioritized, the research team pragmatically collapsed the scale into a binary classification: low importance (1–4) and high importance (5–7). This decision allowed us to distinguish items perceived as meaningful to participants. A more stringent threshold of ≥80% agreement was used for consensus in R2, and items that met this threshold were labelled as important.
We conducted two rounds of the Delphi process, which is generally deemed sufficient.37,38 Subsequent rounds were not conducted as the research team judged that additional data collection would be unlikely to yield additional consensus. In R1, open-text feedback was reviewed by the research team to identify statements requiring clarification, refinement, or consolidation. Suggestions made by participants to include additional items within each domain were also examined, and new statements were created for R2, where applicable. We did not conduct a formal qualitative analysis on the open-ended responses.
Results
A total of 286 RTs participated in R1 and 165 in R2 (Table 1). The mean age of participants was approximately 41 years across both rounds, and the majority identified as cis women (n = 226; 79% in R1; n =118; 72% in R2). Most participants held a diploma (46.9% in R1; 44.8% in R2) or bachelor’s degree (39.2% in R1; 35.1% in R2), with representation from all provinces and territories. The average duration of RT practice was 19.0 years in R1 and 15.2 years in R2, with weekly hours averaging 36.2 and 34.8, respectively. RTs reported working across diverse clinical areas, including in-patient care, community settings, anesthesia assistance, neonatal/pediatric care, education, and management. Participants also represented a range of roles, from frontline clinicians to leadership and educational positions.
Overview of Consensus
In R1, 11 out of 74 statements (15%) reached consensus (≥70% agreement), which we categorized as priorities. After incorporating open-ended feedback, some statements were combined, resulting in 53 statements carried forward. In R2, an additional 11 of 53 statements (21%) achieved consensus (≥80%), which we categorized as important (Table 2). Consensus items spanned all domains except RT Education, which had only one consensus statement after R2. All other domains identified at least three priority items. Figures 2 and 3 show response distributions by domain. Full ranking data for the entire cohort and all subgroup analyses are provided in Supplementary File 2.
Domain 1: System-level impact of RTs
Across both rounds, six items in this domain reached consensus. In R1, three items of the possible 17 (17.6%) were categorized as priorities, which include investigating RTs’ role, practices and impact on patient outcomes and the healthcare system, RT roles for airway management and as rapid response team members and investigating the role, practice and impact of new and emerging RT roles that may facilitate healthcare delivery and decrease system-level burden. Statements that did not achieve consensus still received strong support, with 85% of responses falling within the moderate and high priority categories (Figure 2A).
In R2, another three items of the possible 15 (20%) were categorized as important. The items revolved around evaluating the distinct roles, practices and impact of RTs or AAs in perioperative teams, RTs those caring for multiple patient populations simultaneously and investigating how RTs influence patient safety. Statements without consensus had 51 to 79% of responses categorized within the high importance category (Figure 3A).
Domain 2: Optimizing RT Practices
Across both rounds, eight statements achieved consensus in this domain. In R1, five items of the possible 19 (26.3%) were categorized as priorities. These items included investigating impacts of RTs managing individualized mechanical ventilation, the strategies and impacts of conducting RT assessment of patients in care settings (e.g., primary care clinic, emergency room, in-home), RT-driven protocols, invasive airway management and non-invasive usage in chronic respiratory diseases (e.g., quality of life, healthcare utilization, mortality). The statements that did not reach consensus had approximately 90% of the responses within the moderate and high priority categories (Figure 2B).
In R2, three items of the possible 10 (30%) achieved consensus and were categorized as important. The items were focused on optimizing practices in non-conventional ventilation (and different ventilators), lung mechanic measurements and advanced imaging technologies to support patient care. The remaining statements without consensus had 51 to 75% of responses categorized within the high importance category (Figure 3B).
Domain 3: Scholarship on the RT Profession
Seven statements reached consensus in this domain. In R1, three items of the possible 26 (11.5%) were categorized as priorities. These items included determining the optimal RT to ventilator ratios across practice settings and how these ratios impact patient outcomes, understanding RT recruitment, retainment, work resilience and burnout across different practice settings, and identifying strategies to mitigate them. Statements that did not reach consensus had approximately 87% of the responses within the moderate and high priority categories (Figure 2C).
In R2, four items of the possible 17 (23.5%) achieved consensus and were categorized as important. This included evaluating the RT practice profile, specifically in improving patient outcomes and the perceived RT value by other members of the interprofessional team, RTs role in health policy changes and investigating RTs’ critical and clinical reasoning skills, from development to evolution. The remaining statements without consensus had 53 to 78% of responses categorized within the high importance category (Figure 3C).
Domain 4: RT Education
In R1, no items in this domain reached consensus and could be categorized as a priority. Approximately 80 to 85% of the responses were categorized within the moderate and high-priority groupings across the 12 statements (Figure 2D). In R2, one item of the possible 11 (9.1%) achieved consensus and was categorized as important. This consensus item was focused on evaluating the impact of RT clinical educators. The remaining statements without consensus had 59-79% of responses categorized within the high importance category (Figure 3D).
Subgroup analyses
Survey responses were also stratified by primary practice setting subgroups and statements re-analyzed to identify new or diverging consensus compared to the total cohort. There was a total of eight subgroups represented: 1) in-patient care; 2) community and chronic care; 3) cardiopulmonary diagnostics; 4) anesthesia assistance; 5) management, administration and leadership; 6) neonatal and pediatrics; 7) RT education; and 8) others (e.g., research, industry, government).
The in-patient care subgroup had the largest sample sizes, including 99 (35% of n = 286) and 60 (36% of n = 165) responses in R1 and R2, respectively. The community and chronic care subgroup in R1 had 68 (24%) responses, which dropped to 24 (15%) in R2. The remaining subgroups consistently had 30 or fewer responses for R1 and R2, with the smallest sample size in the neonatal/pediatrics and the other subgroups (both n = 6) in R2.
The number and specificity of consensus statements in R1 and R2 in these subgroups differed from the total cohort. A summary of these differences is shown in Table 3. Many subgroups had greater number of consensus statements compared to the total cohort for that specific Round, and consensus statements also differed. For example, after 2 Rounds of the Delphi, only one RT education statement met consensus by the whole cohort. However, within the education group, five statements for each of the two Rounds were deemed priorities and important. The ranked statements across practice setting subgroups and the differences in consensus statements are detailed in the Supplementary File 2. For each statement, the median, 25th and 75th percentile rankings and distribution of responses by the priority or importance categories are also provided. Additional subgroup analyses (e.g., by provincial/ territorial regions) were not conducted as these subgroup sample sizes were too small to analyze meaningfully.
Discussion
The objective of this modified Delphi study was to identify which previously documented knowledge gaps in RT practice in Canada would be endorsed as research priorities. Reaching consensus suggests that these topics are viewed as the most relevant and impactful by the profession. Of the 74 initial research priorities presented in R1, 11 (14.8%) met the criteria to be identified as priorities, and an additional 11 (20.7%) from the remaining 53 items in R2 were classified as important. These findings represent an important first step toward advancing a focused, profession-driven research agenda.
Historically, much of the research related to RT practice has been led by other health professions,24 which may not fully reflect the nuanced realities or priorities of RTs themselves. By establishing these shared understandings of research priorities, these findings represent an important first step toward advancing RT profession-driven, body of knowledge. Moreover, by formalizing these priorities, this study addresses an important gap and supports alignment of future research with the profession’s evolving roles and needs.13,14,39 Without these lines of inquiry to address the knowledge gaps previously identified, important aspects of the practice and profession of RT are likely to remain underexplored. While some authors have offered insight into the research interests of RTs,40 this study undertook a systematic approach to establish consensus-informed priorities across the RT profession, enhancing the credibility and relevance of the identified topics.
The list of priorities generated in this project reflect the complexity of RT practice and its contextual variability. For example, several priority topics focused on the role of RTs in rapid response teams, airway management, and perioperative services, areas that reflect both the breadth and diversity of RTs role and scopes of practice. These topics also demonstrate the profession’s expanding influence beyond traditional bedside care (e.g., patient wards or in intensive care units),39 highlighting the growing involvement of RTs in emergency response, institutional decision-making, and interprofessional models of care such as primary care settings. For example, although there exist moderate-level evidence linking the implementation of rapid response teams with decreased mortality and non-ICU cardiac arrest rates, it remains unclear whether team composition (specifically the presence of an RT) contribute to these outcomes.41 In addition to clinical topics, workforce sustainability emerged as a priority. Several items that achieved consensus focused on burnout,42,43 recruitment, retention,44 and optimal staffing ratios.45,46 The prioritization of these topics underscores the ongoing pressures RTs face in delivering care within under-resourced or high-stakes environments and reflects a broader trend across health systems to improve workforce well-being and capacity.47,48
Notably, consensus was most difficult to achieve in the RT education domain. This may reflect the broad scope of topics included, ranging from entry-to-practice education to continuing professional development. It may have been challenging to reach agreement on educational priorities across the full cohort of participants because of the wide variation in roles and responsibilities among RTs, with RT education representing a relatively specialized aspect of the profession. Supporting this inference, the subgroup analyses suggested significant variation in the number and types of priorities endorsed across different practice settings. In many cases, subgroups identified different statements as consensus priorities compared to the overall sample. These differences highlight a limitation of using Delphi methodology to seek a singular, profession-wide consensus among a heterogenous group. Multiple authors have questioned the validity of consensus in such contexts, acknowledging that, in general, participants’ opinions tend to shift between rounds.49–51 These results illustrate that future research may benefit from tailoring investigations to reflect the diversity of RT specialization areas (e.g., RT education, neonatal/pediatrics, anesthesia assistance) rather than viewing RT practice as a being entirely uniform in its nature.
This modified Delphi study intentionally deviated from some conventional approaches by implementing a more pragmatic analysis rather than rigidly adhering to convention. For example, during data analysis, we applied an a priori consensus threshold across all rounds.35 In R1, we used a three-category classification to identify priorities, with a 70% consensus threshold. In R2, we observed that most items that had not reached consensus in the previous round remained below the threshold, suggesting stability in participants’ views.35,50 However, no new items met the 70% threshold in R2. Rather than reducing the consensus threshold (an approach often used in Delphi studies to increase yield), we adopted a more conservative strategy: recategorizing responses into two levels of importance and raising the consensus threshold from 70% to 80%. This allowed us to identify items that were still broadly viewed as important, while maintaining a rigorous standard for consensus within a diverse and heterogeneous sample.
Overall, the items identified in this study serve multiple purposes. They may inform the development of research questions for RTs pursuing academic or clinical research, guide the focus of postgraduate education programs, support the design of curricular content and continuing professional development opportunities, or shape policy decisions (e.g., the allocation of research funding, expanding scopes of practice). Additionally, these findings provide a structured foundation for establishing strategic roadmaps to advance the RT research agenda.
Strengths and Limitations
This study has several strengths. The development of survey items was grounded in prior qualitative research and co-constructed by the research team, ensuring content validity and alignment with real-world experiences of RTs. The items reflected diverse domains of practice and were informed by an established process to generate, refine, and pilot test the survey content. However, this study is not without limitations.
Despite our dissemination efforts, the response rate remained low, which may introduce response bias, as those who participated could differ in meaningful ways from those who did not (e.g., those that participated had a vested interest in the topic). In future research, researchers could employ a randomized sample, rather than a convenience sample, to enhance the generalizability of the findings. Additionally, while we had an acceptable sample of participants for R1 (n = 286), there was a notable drop in participation in the subsequent round (n = 165), which may have affected the stability and representativeness of the consensus findings. The subgroup analyses were limited by small and uneven sample sizes across categories, thus limiting the generalizability of their findings. They may, however, be suggestive that RTs working in different settings may hold divergent research priorities, which reinforces the importance of considering practice context in future agenda-setting work.
Finally, while this Delphi study was conducted in Canada with a Canadian RT population, some priorities may be transferable to other jurisdictions with similar scopes of practice. Future research could explore the applicability and resonance of these findings in other national and international contexts to determine their broader relevance.
Conclusion
This study established a prioritized set of profession-driven research priorities and important topics for the advancement of respiratory therapy profession in Canada. By using a modified Delphi study to explore previously identified knowledge gaps, RTs identified 22 items as either being a priority or an important area for future research. These findings offer a foundation for shaping future research, education, and policy efforts that reflect the evolving roles and needs of RTs.
Acknowledgement
We would like to thank Zainab Ahsan, Ryan Duntin and Fred Liang for their support in facilitating the survey preparation and preliminary data analyses. We would also like to thank all participants for providing their time to complete the surveys.
Funding
Funding for this project was provided by the Canadian Society of Respiratory Therapists Strategic Project Funding Grant. The funding body had no influence on the data collection, analysis or writing of this manuscript. MZ is supported by a Banting Postdoctoral Fellowship (#509780) from the Canadian Institutes of Health Research (CIHR).
Competing interests
All authors have completed the ICMJE uniform disclosure form and declare no conflict of interest. MZ is deputy editor of the Canadian Journal of Respiratory Therapy, AW is an associate editor of the Canadian Journal of Respiratory Therapy, SQ and MLN are on the editorial board of the Canadian Journal of Respiratory Therapy. None were involved in any decision regarding this manuscript.
Ethical Approval
This study received research ethics board approval from the Hospital for Sick Children (SickKids, #1000079058) and Ontario Tech University (#16789).
AI Statement
During the preparation of this work, the authors used OpenAI GPT-4o mini to summarize the content of the research protocol and Zaccagnini, et al.,25 only to inform and guide the content of the introduction and methods section of this paper. After using this tool/service, the authors reviewed and edited the content extensively and take full responsibility for the content of the publication.


__modera.png)
__and_*hi.png)
__modera.png)
__and_*hi.png)