Introduction
This study aims to understand how common soft good materials used in infant products impact respiration patterns. According to the American Academy of Pediatrics (AAP), approximately 3,500 infants die of a sleep-related incident each year in the United States.1 Suffocation, asphyxia, entrapment, and sudden infant death syndrome (SIDS) encompass the term sudden unexpected infant death (SUID), and no single factor or condition has been proven to cause SUID. Some research has suggested genetic or brain abnormality factors as increasing risk,2 while other research has found that 72% of SUID deaths occur in unsafe sleeping environments, indicating that suffocation and/or body position play a role.3 In 1992, the AAP recommended that babies sleep on their backs to reduce the risk of SIDS. Two years later, in 1994, the National Institute of Child Health and Human Development launched the Back to Sleep campaign and established what is known as the ABCs of Safe Sleep: infants should sleep alone, on their back, and in a crib. These safe sleep guidelines were advertised as a preventative measure to reduce the risk of SUID. Over 30 years later, even with these well-known guidelines, infants often nap or sleep in commercial products (i.e. swings, rockers, bouncers, etc.), introducing hazards that do not exist in a firm, flat crib environment.
Body position and surroundings both impact respiratory patterns in infants and adults alike. Infants in the U.S. spend an average of 5.7 hours per day in seated and inclined commercial products.4 These products introduce a unique mechanical environment where some infants can achieve a roll or other coordinated movements before they are able to do so on a flat surface, increasing their likelihood of facial interaction with the product.5 Despite being placed supine in these products, infants sometimes roll to the prone position where a hazardous suffocation situation arises (Figure 1). Once prone, facial contact with their nose and mouth on plush soft goods of the product is likely unless the infant can self-correct or has the strength and control to keep their head lifted off the surface for a prolonged period. Some of these products advertise the materials as “safe” or “breathable”, yet quantification of how the materials impact breathing when an infant’s face is in contact is unknown.
In many commercial products, infants are surrounded by fabrics, plush materials, or soft goods that come into contact with their noses and mouths. Infants under six months are more likely to suffer breathing-related injuries caused by suffocation compared to older children, so plush soft goods are a serious concern.6 Yet, there is a lack of understanding of how the material composition of these soft goods impacts breathing. One study on carbon dioxide (CO2) rebreathing induced by crib bumpers concluded that an adequate seal must be made around the mouth and nose such that exhaled gas is directed into, and gas can be inhaled from, the storage medium.7 The materials that make up infant products may be mediums that store this exhaled gas, leading to the potential for CO2 rebreathing.
This is the first study to quantitatively measure the breathing effects of materials in a simulated prone infant scenario. More research into how materials influence breathing is necessary to provide a foundation of knowledge for safer infant product design, with the potential to reduce infant injuries and deaths. Therefore, this study aimed to characterize how common infant soft goods materials influence respiration. We hypothesized that there would be significant increases in end-tidal carbon dioxide (EtCO2) and significant decreases in oxygen saturation (SpO2) when breathing into materials.
Methods
This study was approved by the Boise State University Institutional Review Board (IRB) in compliance with this institution’s Federal Wide Assurance and the DHHS Regulations for the Protections of Human Subjects (IRB24-040, approved date 08 February 2024).
Participants
Healthy adults aged 18-40 were recruited for this Institutional Review Board (IRB) approved study. Those excluded from this study were individuals currently diagnosed with respiratory or neurological conditions. For ethical reasons, using an adult population instead of infants in this study allowed us to extend the trial length and evaluate respiratory patterns from participants with safety and experimental control. Although the use of adults is an important limitation of our study, we expect the results from adults will underestimate the effects we would see with an infant population due to the infant’s increased respiratory vulnerabilities.
Experimental Design
Participants were instructed to lie prone on a bench where the sagittal plane body position was controlled to mimic how an infant would lie if positioned face down (Figure 2A). The bench featured a head pillow with a removable center (Figure 2C). Participants’ faces were in contact with the removable center, ensuring their nose and mouth were in contact with only this portion of the pillow. The room temperature of the lab was maintained between 20 and 22 degrees Celsius, and the humidity was between 40 and 60%.
Material selection
The four selected materials were chosen based on the typical composition of infant products like bouncers, swings, rockers, and car seats: 100% cotton, 100% polyester, 50% cotton 50% polyester, and 10% spandex 90% polyester.8 Most infant products contain a variety of these materials, with 100% polyester being the most common of the four in a subset of products we previously evaluated.8 Soft goods are usually composed of one of these selected materials covering a padding. To mimic these soft goods compositions, selected materials were cut into equal 17 x 10-inch rectangles that could completely wrap around polyester fill (5.5 x 5.0 x 4.5 inches). This allowed materials to be placed in the head pillow’s removable center (see Figure 2C).
Equipment
Respiratory data was collected using a Capnostream 35 Portable Respiratory Monitor. A side-stream nasal cannula collected respiratory rate and EtCO2, while the finger probe collected heart rate and SpO2. The two primary variables of interest were EtCO2 and SpO2 because they are key measures in evaluating suffocation risk, and we also collected respiratory and heart rates to compare with previous literature.9–11 We monitored if participants’ EtCO2 dropped below 2% (15 mmHg) or exceeded 8% (60 mmHg), and when SpO2 fell below 85% or exceeded 100%; trials were stopped if EtCO2 or SpO2 stayed in those ranges for more than five seconds.
Procedure
Individuals first provided written consent. We then collected demographics and health behaviour characteristics using a self-reported questionnaire. Once fitted with the nasal cannula and finger probe, participants completed seven 10-minute trials with a 2.5-minute break between trials. Participants were asked to breathe normally through their noses for the seven trials. The first, middle, and last trials served as baseline measurements where no material was in the head pillow hole, and participants could breathe freely in the testing position. The four remaining trials tested the four materials of interest and placed them in the spot of the removable center, so participants were only breathing into the material selected for that specific trial. The order of testing the four materials was randomized for each participant. After each of the seven trials, participants were asked to rank on a scale of 1-10 how difficult it was to breathe, where 1 meant no difficulty breathing and 10 meant the most difficulty breathing. Participants could end trials at any time they felt too uncomfortable, dizzy, or struggled to breathe to the point of unease.
Questionnaire
Questions about health status and respiratory conditions were asked to evaluate their potential connection to respiratory compromise.12 These questions included smoking status, physical activity per week, and history of asthma, sleep apnea, and snoring.
Statistical analysis
Data analysis was performed in SPSS. A One-Way Repeated Measures ANOVA (p < 0.05) with Tukey post-hoc tests were used to determine differences in carbon dioxide output, oxygen saturation, respiratory rate, and heart rate mean values in the testing conditions. An average of the three baseline trials was taken for a single baseline value for each participant. The mean values for EtCO2 and SpO2 were also calculated and normalized to the mean baseline for comparison. The percent change from the mean baseline was calculated for each material. A two-tailed t-test of equal variance was used to determine statistical differences between participant rankings (p < 0.05).
Results
The mean age of the participants was 22.5 ± 3.2 years (4M/5F). The mean BMI was 21.7 ± 3.3 kg/m2, and 77% reported engaging in regular exercise, 22% reported a history of asthma, and 22% reported a history of snoring (see Table 1). Participants consistently ranked the baseline a “1” for no trouble breathing, and each material trial significantly greater than the baseline (see Table 2). In all trials collected, none were stopped early due to EtCO2 and SpO2 readings in the alarming range (if EtCO2 dropped below 2% or exceeded 8%, and if SpO2 dropped below 85% or exceeded 100% for more than 5 seconds). One participant chose to end all four of their material testing trials before the 10-minute mark due to self-reported “extreme difficulty breathing” (cotton; 3 minutes, 50/50; 2 minutes, polyester; 1 minute, and spandex; 2 minutes 30 seconds). This participant’s respiratory outcome data were therefore excluded from the quantitative results.
Participant baseline EtCO2 and SpO2 levels were 38 mmHg ± 2.9 and 97.4 ± 1.1, respectively. There were no significant differences between the three baseline trials for each participant. For each material condition, there was an increase in mean EtCO2 output and a decrease in mean SpO2 levels from the baseline condition. Participant baseline respiratory rate and heart rate levels were 12.4 ± 3.4 breaths per minute and 72 ± 11.2 beats per minute, respectively. For each material condition, there was a decrease in mean respiratory rate and an increase in mean heart rate from the baseline condition, though significance was not reached (Table 2).
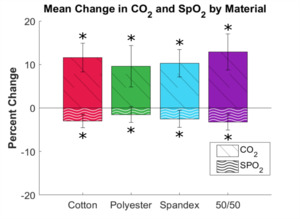
There was a statistically significant difference in the mean EtCO2 when breathing under each condition (p = 0.012). From the Tukey post hoc test, there was a statistically significant difference in EtCO2 during the baseline condition and cotton material (p = 0.035) and the baseline and 50/50 material (p = 0.010). However, differences between the baseline and polyester material (p = 0.12) and the baseline and spandex material (p = 0.075) did not quite reach significance. There were no significant differences in EtCO2 between the materials.
There was a statistically significant difference in the mean SpO2 when breathing under each condition (p = 0.001). In the post hoc analysis, there was a statistically significant difference in SpO2 during the baseline condition and cotton material (p = 0.002), the baseline and spandex material (p = 0.016), and the baseline and 50/50 material (p = 0.001). However, there were no differences between the baseline and polyester material (p = 0.286). There were no significant differences in SpO2 between the materials.
There was no statistical significance in the mean respiratory rates between the baseline and four material conditions (p = 0.381). There was a statistically significant difference in the mean heart rates between the baseline and four material conditions (p = 0.008). In the post hoc analysis, there was a statistically significant difference in heart rates during the baseline condition and cotton material (p = 0.029), the baseline and polyester material (p = 0.042), the baseline and spandex material (p = 0.046), and the baseline and 50/50 material (p = 0.009). There were no significant differences in heart rates between the materials.
Mean and standard deviations of the percent change in EtCO2 and SpO2 for each material from the baseline were calculated (Figure 3).
Discussion
This study aimed to determine how materials found in infant products influence respiration patterns of adults in the prone position. We hypothesized that there would be significant increases in EtCO2 and significant decreases in SpO2 when breathing into the soft goods. Overall, we found increases in end-tidal carbon dioxide and decreases in oxygen saturation for each material, though significance varied. The 100% cotton and 50/50 cotton/polyester materials both resulted in significant changes in EtCO2 and SpO2, while the spandex resulted in only a significant change in SpO2, and no significant changes were detected for the 100% polyester material.
Commercial characterizations of soft goods typically emphasize apparel applications, with limited attention to how these materials behave near an infant’s nose and mouth during sleep. While 100% cotton and 50/50 cotton/polyester blends are often described as “breathable” and moisture-absorbing due to their natural fibre content, participant feedback and respiratory outcomes in face-down scenarios suggest a disconnect between these marketed properties and actual performance in respiratory-related contexts. The weave and thickness potentially created a more difficult environment to breathe through directly. Some participants commented that the 10% spandex material was the most breathable of the four tested, likely due to its blend with other materials. Spandex on its own is not a very breathable material because it traps heat and moisture. In a blend, like the material we tested and most athletic attire, it becomes more ventilated for air circulation.
The 100% polyester is the most common material in many infant products, yet it is typically labelled as less breathable for clothing. Participants commented on the difficulty of breathing into the 100% polyester, possibly because of how it reacts to warm or humid conditions. Breathing directly into the material for 10 minutes created a hot, humid environment that made participants feel difficulty during breathing. However, the EtCO₂ and SpO₂ measurements did not reflect this subjective experience.
In our study, participants responded on a Likert scale of 1-10 for how difficult it was to breathe, where 1 meant no difficulty breathing and 10 meant the most difficulty breathing. They consistently ranked the baseline a “1” and each material trial significantly greater than the baseline (cotton: 6.1 ± 1.9, polyester: 6.4 ± 2.2, spandex: 5.5 ± 1.8, and 50/50: 6.6 ± 2.0; p < 0.05). The respiratory data for the baseline trials showed no changes in respiratory outcomes, whereas in the material trials, we saw some significant increases in EtCO2 and some significant decreases in SpO2. Participant comments like “hyper focused on big, long breaths” or “felt dizzy from difficulty inhaling” on these material trials also aligned with the significant changes we saw. A single survey question is unlikely to fully capture the concept being assessed, but our unique quantitative data and participant comments provide context for the respiratory results.13 Participant feedback regarding trial difficulty could not otherwise be fully assessed.
We utilized capnography to measure key respiratory patterns in our study. EtCO2 monitoring is a noninvasive technique that measures the partial pressure or maximal concentration of carbon dioxide at the end of an exhaled breath, which is expressed as a percentage of CO2 or mmHg. The normal values are 5% to 6% CO2, equivalent to 35-45 mmHg.14 Measuring this gives a vital sign for ventilation and perfusion because the volume of CO2 excreted by the cardiorespiratory system is a sensitive indicator of ventilation efficiency, pulmonary perfusion, and cardiac output.15 In our study, the mean baseline and means for each material were all within the normal 5% to 6% range, but there were large standard deviations; therefore, some participants experienced abnormal CO2. We saw significant increases when breathing into the cotton and 50/50 materials.
Capnography measures oxygen saturation through pulse oximetry using a colorimetric light sensor attached to a finger. The amount of oxygen in the blood, or blood oxygen saturation level, is defined as the fraction of oxygen-saturated hemoglobin in red blood cells compared to the total amount of hemoglobin.9 In adults, readings between 95% and 100% are considered normal; readings between 90% and 95% are considered mildly hypoxic, and a level of 90% or below indicates hypoxemia that needs to be treated quickly.9 Like adults, healthy infants have baseline SpO2 levels greater than 95%. Previous longitudinal observations of SpO2 changes in infants identified relevant correlations with age, apnea, and sleep position.10 In our study on adults, the mean baseline was within the normal 95% to 100% range, while the cotton and 50/50 materials were significantly lower than the baseline. This significant decrease in SpO2, along with the significant increases in EtCO2 for cotton and 50/50, substantiates the dangers that soft goods commonly found in commercial products pose to infant respiration. These results also strengthen the established concern that soft bedding, which often is composed of the materials in our study, can create a hypercapnic and hypoxic microenvironment for infants, a known risk factor for SIDS.
Gas exchange with the environment is an important consideration for impact of respiration. Patel et al. measured concentrations of inspired CO2 and O2 to evaluate rebreathing or abnormal exchange of gases while breathing into bedding.11 End-inspiration CO2 rose by an average of 28.7% after placement of a silk cloth around the face in 11 prone infants, where we found a rise of an average of 12.9% inspired CO2 in adults after lying prone on the 50/50 material for just 10 minutes. The larger increase in EtCO2 that Patel et al. found in infants demonstrates how microenvironments can significantly influence infant safety. With their limited motor control, lower strength, and unpredictable arousal responses, infants are likely to show higher increases in EtCO2 if they encounter these materials in their environment than the adults of our study did, especially when considering a period of more than 10 minutes. The abnormal gas exchanges caused by soft goods increase the likelihood of a hypercapnic or hypoxic event in an infant. When prone in an infant product with soft goods, the environment around the face tends to conform to the face, forming a concave “bowl” shape. This occurrence further promotes rebreathing of the expired respiratory gases. When an infant is face-down, the type of sleep surface they lie on has proven to have a profound effect on rebreathing of carbon dioxide.16 Previous work by Carleton at the Consumer Product Safety Commission (CPSC) confirmed this effect, leading to the recall and ban of certain materials and products for use with infants, like sheepskins and bean-bag pillows.17 Infants are vulnerable to sleep-related risks when placed in these unsafe microenvironments, where factors like bedding and lying position can increase the risk.
Adequate oxygenation is important for all infants, but specifically for those at higher risk for respiratory problems, such as preterm babies or those with medical concerns. In one study, preterm infants (2-6 months of age) experienced falls in SpO2 to 80% for longer than 4 seconds, whereas these episodes were rare 6 weeks later.18 In their first year of life, all infants are vulnerable, but preterm infants are particularly susceptible to respiratory complications. Infants with chronic lung disease (CLD) are more at risk of SIDS due to their vulnerable respiratory systems. The importance of removing soft goods from the sleeping environment is amplified for these two vulnerable populations, where sufficient oxygenation is crucial to their survival in their first year of life. Our study demonstrates that some soft goods reduce adults’ SpO2 levels significantly, in a few trials to as low as 91%. The literature suggests that even values around 89-92%, which are considered adequate for older children and adults, may not be sufficient for infants with CLD.18 The longitudinal study of healthy infants during their first six months of life reported a median baseline SpO2 of 97.9%.10 Healthy or vulnerable infants should maintain a baseline SpO2 of at least 95%. Our findings in adults are even more concerning for infants with greater vulnerabilities after birth.
Heart rate is related to the work the body is doing to maintain function. Our adult population’s heart rate increased as they lay prone with their face in the materials. During our study, we observed a relationship between perceived increased work of breathing through the Likert scale results and increased heart rate. The heart rate for each material was significantly higher than the baseline condition, though adult participants could comfortably remove their faces from coverage at any time during our controlled experiment. However, this environmental risk would be far more dangerous for infants, who have a reduced ability to move away from the hazard.
Increased CO2 is a physiological stimulus that leads to a stereotypical arousal response that relieves the buildup of EtCO2 and refreshes the inspired oxygen supply for infants.19–26 This response is necessary to protect infants from respiratory hazards associated with lying prone. When infants sleep in the prone position, the stimuli evoking arousal are increased CO2 and/or decreased O2.27 In our study, participants experienced increased CO2 and decreased O2 when breathing into the materials. As adults, our arousal response is more developed, and our muscles are more capable of preventing accidental suffocation in the prone position. But studies have shown that spontaneous and induced arousals during sleep are decreased in SIDS victims,28–33 and infants in general have a less robust respiratory response to hazardous situations. When infants are prone and surrounded by soft goods in their sleeping environment, these two factors alone can prevent effective arousal. Infant arousal begins with the occurrence of a sigh and is typically followed by some head movement, but facial occlusion from a soft or plush microenvironment can reduce an infant’s ability to produce sighs for arousal or move from a dangerous position and may ultimately lead to respiratory distress.
Previous research has shown that body position influences respiration along with the environment. A review article on the physiological studies in SIDS research of prone versus supine sleep found that in the prone sleep position, there is reduced arousal and poorer ventilatory and airway protective responses and likely decreased mechanical efficiency of the diaphragm. Each of these factors further increases the exposure to respiratory stress, like rebreathing, that can be a key factor in the cause of SIDS.34 Because younger infants lack the motor control and strength to sit upright, the angle and design of the product in which they are placed directly affect their posture and thus their ability to breathe normally. Both head/neck and trunk flexion negatively impact breathing,35–37 and we have previously shown that inclined seated products increase both head/neck and trunk flexion.5,8 When infants are prone in inclined seated products, they require increased muscle activity in their abdominals to maintain their position and breathe.5,8,38 Abdominal muscles are critical in performing the work of breathing, so overuse of these muscles reduces the ability to breathe normally and can lead to early fatigue.
Limitations
This study was not without limitations. The side-stream nasal cannulas are affected by mouth breathing, so participants were asked and encouraged to breathe through only their noses, though we did not assess the presence of accidental mouth breathing. Nasal cannula sampling ports can be compromised by kinking, water precipitation, or obstruction at the opening by nasal soft tissue or mucus.39 Mouth breathing during sleep is uncommon, and nasal breathing is preferred by infants.40 Data in our study were collected from healthy young adults, and results cannot fully explain infants’ reactions to breathing into these materials, though we expect that infants’ breathing will be even more negatively affected, considering their underdeveloped respiratory systems. With limited research on common infant product materials’ effect on respiration, the results of our study demonstrate how materials impact essential respiratory outcomes in a short time of only 10 minutes.
Conclusion
This study demonstrates how common soft goods materials used in infant products negatively affect breathing in healthy adults. The results show that EtCO2 increased but was still within the normal range, and oxygen saturation dropped below a normal range for all tested materials. Although not all materials showed significant changes in both metrics, an increase in carbon dioxide and/or a decrease in oxygen saturation over a longer period is enough to put infants at increased respiratory risk. Further research with an adult manikin and a scaled-down model with an infant manikin will further substantiate these initial findings.41
Well-informed public health guidelines from the AAP in 2022 advise parents on safe sleep recommendations. Infants should always be placed on a firm, flat surface with no soft bedding on or around them to sleep. Yet, infants inevitably fall asleep in their car seats or other inclined seated products that often contain soft goods. We suggest that breathing-related measures be quantified for soft goods that are likely to be in contact with an infant’s face when infants are awake or asleep. Manufacturers and caregivers should make conscious efforts to limit the risk of infants’ faces contacting soft goods materials that inhibit normal breathing, to reduce the risk of respiratory-related injury or death.
Contributors
Contributor roles are defined as follows using CRediT: HO - conceptualization, formal analysis, investigation, methodology, project administration, visualization, writing original draft, writing review & editing; AB - conceptualization, investigation, methodology, software, visualization, writing review & editing; MK - supervision, validation, writing review & editing; CS - supervision, validation, writing review & editing; EM - conceptualization, formal analysis, funding acquisition, resources, validation, writing original draft, writing review & editing. All authors have approved the manuscript and agree with its submission to CJRT.
Funding
National Institute of General Medical Sciences, #P20GM148321.
Conflicts of interest
All authors have completed the ICMJE uniform disclosure form and declare no conflict of interest.
Ethical approval
This study was approved by the Boise State University Institutional Review Board (IRB) in compliance with this institution’s Federal Wide Assurance and the DHHS Regulations for the Protections of Human Subjects (IRB24-040, approved date 08 February 2024).
AI Statement
No generative AI or AI-assisted technology was used to generate this manuscript or its content.

_on_a_flat__firm_crib.png)
_experimental_setup_with_a_participant._(b)_capnostream_components__including_the_nasal.png)
_on_a_flat__firm_crib.png)
_experimental_setup_with_a_participant._(b)_capnostream_components__including_the_nasal.png)
