Introduction
High-risk newborns are more susceptible to muscle fatigue, need for ventilatory support, hospitalization and respiratory physiotherapy due to the small number of alveoli, more horizontal and cartilaginous ribs, higher airway resistance, and higher compliance of the rib cage.1,2 The main goal of respiratory physiotherapeutic interventions is to improve respiratory function to facilitate gas exchange and adjust the ventilation-perfusion ratio.3
These interventions are stratified into conventional (i.e., older) and non-conventional or current techniques. Conventional techniques comprise chest vibration, percussion or tapping, and postural drainage, in which chest vibration and tapping make use of thixotropy, promoting the propagation of mechanical waves in the newborn’s chest, while postural drainage presents the physical characteristic of gravitational action for the mobilization of secretions.3,4 The non-conventional techniques include expiratory flow acceleration, slow and prolonged exhalation, assisted autogenic drainage, total slow exhalation with open glottis, and thoracoabdominal rebalancing. These techniques are characterized as passive approaches, with distinct objectives: some aim at mucociliary clearance and secretion mobilization (expiratory flow acceleration, slow and prolonged exhalation, assisted autogenic drainage, total slow exhalation with open glottis), while others focus on muscle synergy.3,4
Both conventional and non-conventional respiratory physiotherapy techniques are commonly used in Neonatal Intensive Care Units (NICU). Studies suggest benefits for secretion mobilization3–6 and thoracoabdominal stability.6–8 However, there is still controversy regarding their effects on respiratory mechanics, pain, and vital parameters in newborns,5–12 which influences the choices of which respiratory physiotherapy techniques to use for clinical management in newborns.
There is a lack of clinical trials comparing conventional and non-conventional respiratory physiotherapy in newborns. Additionally, no systematic reviews comprehensively evaluate their efficacy, underscoring the need for more robust comparative studies and reviews to improve evidence-based practices and outcomes for newborns. In this context, this systematic review was conducted to evaluate the effects of conventional and non-conventional respiratory physiotherapy on pulmonary mechanics, vital parameters and pain in newborns admitted to the NICU.
Methods and Analysis
This systematic review was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.13 The protocol for this review is registered with the PROSPERO International Prospective Register of Systematic Reviews (CRD42019139365) and previously published. The protocol has previously been published.14
Eligibility Criteria
Types of studies
Following the PRISMA recommendations for systematic reviews evaluating the effectiveness of interventions, only randomized controlled trials were included.13 Although this more restrictive inclusion criterion may have contributed to fewer eligible studies, this design is considered the gold standard for assessing intervention effectiveness, as it minimizes bias through random allocation and allows for greater control over confounding variables.13 Studies that were incomplete, did not report the outcomes of interest, or were not available in full text were excluded. Additionally, all other study designs (e.g., observational studies and case reports) were excluded to ensure consistency in the level of evidence analyzed.
Types of participants
Studies conducted with newborns of both sexes, aged 1 hour to 28 days, admitted to the NICU and either on mechanical ventilation or not, were included. Studies with newborns who had structural changes (e.g., chest wall deformities, abdominal pathologies, and heart disease) were excluded.
Types of interventions
Human studies that compared conventional techniques (e.g., vibration, or vibrocompression, percussion, and postural drainage) with non-conventional physical therapy techniques (e.g., autogenic drainage, increased expiratory flow, prolonged slow expiration, and thoracoabdominal rebalancing) were considered for inclusion in the study. The description of the techniques can be found in the study protocol.14
Types of outcome measures
The primary outcomes considered were: 1) lung compliance and airway resistance, (evaluated in the mechanical ventilator using the following formulas: Cdyn = VT / PI - PEEP; Cstat = VT / Pplateau - PEEP; Craw = PI - Pplateau / inspiratory flow); 2) Lung volumes and capacities, assessed by pneumotachograph coupled to a flow transducer; and 3) Thoracoabdominal synchrony, assessed by rater observation, Silverman Andersen respiratory severity score, and methods for assessing thoracoabdominal motion (e.g., plethysmography and biophotogammetry).
The secondary endpoints considered were: 1) Respiratory discomfort: assessed by any instrument that evaluated respiratory discomfort, and the data were expressed in dichotomous responses (yes or no for respiratory discomfort); 2) Pain: the instruments used to assess pain were not limited. All pain assessment scales were considered, and the data were expressed in dichotomous answers (yes or no for the presence of pain); 3) heart rate (HR): assessed by multiparameter monitors; respiratory rate (RR): total respiratory incursions in one minute, assessed visually or by multiparameter monitors; 4) peripheral oxygen saturation (SpO2): assessed by pulse oximetry or multiparameter monitors.
Information sources
Research strategy
The initial search was conducted between September and October 2022, covering all records available in the databases. Additional searches were performed in January 2023 and November 2024 to update the data and ensure the possibility of including more recent studies. The searches were conducted in the following databases: PubMed, LILACS, SciELO, Science Direct, Cochrane Library, and Web of Science databases. Also, manual searches of the references of the included studies were performed.
This review used terms indexed in DeCS/MeSH, health science descriptors, and free terms available in fully published articles. Combinations of the terms using the Boolean operators OR and AND, as well as truncation operators, were also used. The main terms used for the searches were: Newborn AND Physical Therapy Modalities OR Respiratory Therapy AND Respiratory Mechanics OR Lung Volume Measurements OR Heart Rate OR Respiratory Rate; “Newborn Infant” AND “Physiotherapies” OR “Physical Therapy Modalities” AND “Breathing Mechanics” OR “Breathing Mechanic” OR “Lung Volume Measurement”. The supplementary material provides a detailed description of the search strategies.
Study selection
The results were imported into Mendeley’s reference management tool (https://www.mendeley.com) for duplicate removal. Subsequently, the references were exported to Rayyan QCRI (https://www.rayyan.com) for screening. Two researchers (AMN and ATCS) independently assessed titles and abstracts. In cases of disagreement, a consensus meeting was held between the two reviewers to resolve conflicts. The lead reviewer (AMN) made the final decision if consensus was not reached. The same process was followed during the full-text screening phase. Although AMN participated in both screening and consensus discussions, efforts were made to minimize potential biases by involving a third independent reviewer (SAP) in all stages of screening to ensure data integrity.
Data extraction
Data were extracted from all included studies using a proprietary form. Two authors (AMN and MFPC) performed the data extraction, and two others (KSM and SAP) verified the data accuracy and completeness. [Supplementary Material]
Evaluation of methodological quality
Two reviewers (AMN and ATCS) independently assessed the risk of bias using the following domains of the PEDro scale: eligibility criteria, random allocation, hidden allocation, baseline comparability, participant blinding, therapist blinding, rater blinding, adequate follow-up, intention-to-treat analysis, between-group comparisons, and measures of variability. The total scale scores range from 0 to 10, and the risk of bias was interpreted as high (0 to 3), moderate (5 to 7), or low (8 to 10).15
Data analysis
The characteristics of the interventions are described and presented as mean and standard deviation, median, and interquartile range. It was not possible to perform a meta-analysis because data on the comparisons between groups were not available using the same metrics for comparison.16,17
Certainty of the evidence
It was not possible to perform the evaluation of uncertainty around the evidence with the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) because one of the items to be evaluated is the magnitude of the effect, which is seen using meta-analysis.18
Results
Characteristics of Eligible Studies
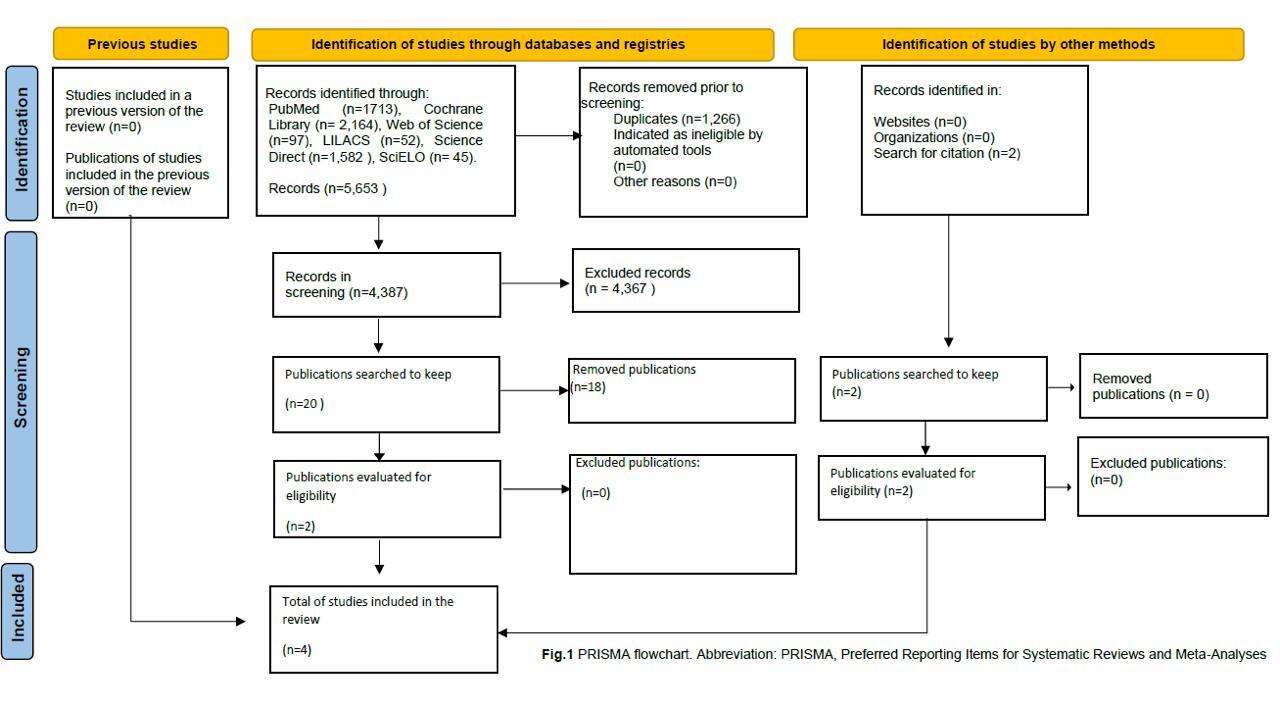
The search resulted in 5,653 articles. After the exclusion of duplicates, 4387 articles were analyzed. Twenty (20) were considered possibly eligible, but only two were included after full reading. Next, manual searches were performed on the references of the included articles, resulting in two additional articles. The flowchart in Figure 1 summarizes the information from the search strategy and study selection.
Participants’ characteristics
The included studies evaluated 205 NB, 54.9% were female, with an average age ranging from 11 to 29 days old and birth weight from 1105g to 2980g. A detailed description is available in Table 1.
Characteristics and Protocols of the Interventions
All the studies made use of the vibrocompression technique associated with other techniques as part of the intervention protocol in one of the groups.16,17,19,20 Thoracoabdominal Rebalancing was cited in two studies as a protocol of non-conventional physiotherapy.19,20 The other studies used the Lung Squeeze technique (manual hyperinflation with manual resuscitator bag)16 and accelerated expiratory flow17 as part of non-conventional physiotherapy.
Regarding the duration of treatment, the follow-up time for evaluation ranged from a single session19,20 to three days16,17 and the time for each session was between 10 and 20 minutes in the four studies.16,17,19,20 The characterization of the interventions is shown in Table 2.
Wong et al.16 made use of the percussion and vibration technique, which was performed with the newborn in a postural drainage position, alternating sides, in a horizontal position without head elevation, compared to lung squeeze in combination with sustained manual chest compression for 5 seconds, followed by a light and gentle release.16
In the research by Antunes et al,17 the newborn in the control group received the slow expiratory flow acceleration technique, in the supine position for 15 minutes, with the therapist’s hands positioned on the lower ribs and cubital border on the supra-breast line. The experimental group received postural drainage and tapotage positioned in right and left lateral decubitus for 5 min on each side. They were subjected to chest vibration for another 5 minutes in the supine position.17
Martins et al.19 tested two different conventional physical therapy protocols. One group was tested using a mechanical vibrator, followed by light manual chest compression, and a second experimental group received the thoracoabdominal rebalancing method. Assessment of vital parameters and pain was performed at three different times (T1= initial assessment; T2= post-immediate assessment; T3= post-15 min assessment) for all groups.19
The study by Oliveira et al20 used different manual therapy techniques in the control group. In this group, newborns received passive expiratory therapy, thoracic expiratory vibration, thoracic vibrocompression, and prolonged slow expiration. They were compared to newborns in the experimental group, who received lower abdominal supports, thoracoabdominal support, iliocostalis support, and inspiratory assistance lasting 15 min each intervention.20
Primary outcomes
No included studies evaluated lung mechanics variables, such as compliance, resistance, lung volumes, and capacities, and thoracoabdominal synchrony.
Secondary outcomes
None of the included studies evaluated respiratory distress. Regarding pain, two studies assessed newborn pain after physiotherapy interventions using the Neonatal Infant Pain Scale (NIPS), Neonatal Facial Coding System (NFCS), and Premature Infant Pain Profile (PIPP). Both studies demonstrated significant pain reduction in newborns across intervention groups. One study showed significant pain reduction measured by both NIPS (p = 0.011) and PIPP (p = 0.005), while the non-conventional physiotherapy group showed improvement only in NIPS scores (p = 0.037); no changes were observed using the NFCS.19
Another study assessed pain via NIPS and found that both conventional and non-conventional physiotherapy significantly reduced pain (p = 0.001).20 Considering HR, among four included studies, only one reported an increase in HR at the first (p = 0.040) and second minute (p = 0.033) following conventional physiotherapy,17 the remaining studies found no significant changes.16,19,20 RR was significantly reduced after both physiotherapy techniques in one study (p < 0.001),20 with two other studies reporting reductions that were not statistically significant.17,19 One study did not report RR outcomes.16
Regarding SpO₂, two studies reported increases following physiotherapy.17,20 Elevated SpO₂ was observed after conventional physiotherapy at the first (p = 0.028) and second minute (p = 0.035), and after non-conventional physiotherapy at the first (p < 0.001) and second minute (p = 0.010).17 Significant improvements in SpO₂ for both conventional and non-conventional physiotherapy groups were also reported (p = 0.003).20 Table 3 presents the results of the secondary outcomes.
Evaluation of the methodological quality of the included studies
According to PEDro scores, one of the four studies showed moderate risk,20 and three low risk.16,17,19 The characterization of the studies’ scores is described in Table 4.
Discussion
The results of this systematic review indicate that both conventional and non-conventional respiratory physiotherapy techniques did not negatively affect vital parameters (HR, RR, SpO2) and pain in newborns. Only one study17 demonstrated a significant increase in HR following conventional physiotherapy. Additionally, it was observed that respiratory physiotherapy techniques led to a reduction in pain and an increase in SpO2 in newborns.19 However, no studies have specifically evaluated lung mechanics or respiratory distress. The scarcity and variability of available research make it challenging to accurately assess the effects of these interventions on these outcomes. It is also important to highlight that these results cannot be generalized due to the limited number of included studies.
The study by Antunes et al. highlights that conventional chest physiotherapy techniques appear to increase SpO₂ and HR levels, but only when applied to newborns after extubation.17 This outcome was attributed to the use of tapotage, a manual chest physiotherapy technique involving rhythmic percussion on the thoracic wall intended to mobilize bronchial secretions, as one of the interventions in the protocol.17 Tapotage has also been associated with an increased perception of pain,17 which may, in turn, contribute to the elevation in HR.1 Being aware of this analysis is important, since increased HR is an indication of increased pain sensation and can compromise the overall metabolism of the newborn.21
Stabilizing SpO2 and HR seems to be a common outcome after vibrocompression, expiratory flow and/or postural drainage techniques.21,22
Despite these studies not showing negative effects, it’s important to emphasize that the use of the prone position may reduce SpO2. This is because when performing this technique, the newborn should be positioned head-down, where the airways have a reduced lumen compared to the head-up position. Another point is that the newborn has more cartilaginous ribs and a softer thorax, which implies greater airway closure compared to an adult, in addition to the diaphragm working against gravity, which can lead to a reduction in saturation.
Two studies conducted between 2014 and 2015 demonstrated that although HR did not change after the application of vibrocompression and postural drainage22 or increased expiratory flow and vibrocompression,21 SpO₂ and RR remained stable. However, in both studies, pain sensation was not assessed or controlled.
Other studies have investigated pain-related outcomes following the application of conventional and non-conventional respiratory physiotherapy techniques, generally reporting favourable results.19,20 It is important to highlight that increases in pain were predominantly associated with invasive procedures, such as tracheal suctioning, rather than the physiotherapy maneuvers themselves. For example, an integrative review23 indicated that vibrocompression may be potentially painful, while techniques such as postural drainage, passive manual expansion, and lung squeezing appear to be well tolerated. Additionally, a study conducted in preterm newborns showed that the increase in pain occurred specifically after tracheal suctioning, highlighting the differentiated impact of the procedures.24 These findings suggest that although certain respiratory physiotherapy techniques are generally safe and not painful, the associated invasive procedures may significantly contribute to discomfort in newborns. The present review adds to this body of knowledge by clarifying the specific sources of pain related to respiratory therapy in newborns, emphasizing the need for targeted pain management strategies during invasive procedures.
The results of this review point to the scarcity of RCTs in NB with outcomes related to lung mechanics after performing respiratory physiotherapy techniques. In addition, the results of the included studies suggest that respiratory physiotherapy techniques do not promote changes in vital signs and pain in NICU newborns.
Due to the heterogeneity of the results, it was not possible to perform a meta-analysis of the studies included in this review. Some studies did not provide the mean and standard deviation of the evaluated variables.16,17 We contacted the main authors by e-mail, but did not get a reply.
The lack of studies evaluating lung mechanics after the physical therapy protocols employed is another important limitation. There is no way to understand the real effects of respiratory physiotherapy on this variable, considering lung volumes and capacities, and thoracoabdominal synchrony in NB.
A study published in 2017 by Carvalho et al. presents results involving lung mechanics and respiratory discomfort.25 Although the study evaluated lung mechanics and respiratory distress, it was not possible to include it in our review, since slow and prolonged expiration is categorized conventional respiratory physiotherapy technique, which was not considered by our review. New studies, comparing conventional versus non-conventional respiratory physiotherapy techniques, should be encouraged.
Some authors did not report the results of the interventions quantitatively, even after contacting them via email, which hindered the observation of data transparency.
Strengths and limitations
This review systematically synthesized evidence regarding the effects of respiratory physiotherapy interventions on vital parameters and pain in newborns, adhering to the international PRISMA guidelines to ensure the rigour and reliability of the findings. The results provide valuable insights for researchers, clinicians, and physiotherapy students, irrespective of their direct involvement in the neonatal field. However, the limited utility of these findings should be acknowledged, as the inclusion criteria were restricted exclusively to randomized controlled trials, which may have excluded relevant evidence and limited the comprehensiveness of the review. The unavailability of post-intervention data and how the variables were reported made it difficult to prepare a meta-analysis.
Conclusion
Both techniques of respiratory physiotherapy (conventional and non-conventional) did not promote negative effects on vital parameters and pain in newborns admitted to the NICU. It is worth pointing out the lack of studies and the existing variability that make a more detailed analysis of the results difficult.
We encourage the development of more clinical trials that can comprehensively evaluate lung function, taking into consideration lung mechanics, respiratory distress, vital parameters, and pain, comparing the before and after interventions, in the short and long term.
Contributors
All authors contributed substantially to the study design, development of the inclusion criteria, and search strategies. AMN developed, designed, and registered the protocol in the PROSPERO database and final review. SAP, ATNSFF, KSM, and IGA provided critical information and reviewed the review. All authors have read and approved the final version of the review.
Financing
The study was funded by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) - Brazil. AMN received a CAPES grant under Financial Code 001.
Conflicts of interest
The authors declare that there are no conflicts of interest.
Ethical approval
PROSPERO Registration Number: CRD42021266729.
AI Statement
No generative AI or AI assisted technology was used to generate this manuscript or its content.