Introduction
Chronic obstructive pulmonary disease (COPD) ranks among the highest burdens of disease globally, with mortality rates consistently among the top three.1,2 It is characterized by chronic inflammation affecting both small airways and lung parenchyma. Key features of COPD include airflow limitation and a decline in exercise capacity, even in mild cases.3 Pulmonary rehabilitation is widely recommended for COPD patients to enhance exercise capacity, improve dyspnea, and improve overall quality of life.4
However, patients with COPD often stop exercising for various reasons, with ventilatory limitation being a major factor.5,6 The underlying concept is as follows. Pathological changes in COPD reduce the lung’s elastic recoil and cause airflow limitation. This results in intrinsic PEEP occurring in the more peripheral airways, especially during forced expiration, such as during exercise. Consequently, dynamic airway compression occurs, leading to air trapping and the development of dynamic hyperinflation (DH).7 This, in turn, reduces the operational lung volume and increases dyspnea. Previous literature has reported that DH is the main determinant of dyspnea and impairs exercise capacity.8 Dynamic pulmonary hyperinflation can be determined by measuring the decrease in inspiratory capacity (IC).9
Therefore, any intervention method that prevents and/or reduces DH is essential. Positive expiratory pressure (PEP) breathing in COPD, especially when incorporated during exercise, has been a longstanding focus in pulmonary rehabilitation. PEP counteracts the airway’s collapse, disrupting the vicious cycle of air trapping and DH.10
PEP devices can be categorized into two types. The first type, flow-independent PEP devices, uses either a spring-loaded resistance or a column of water to provide a minimum of selected PEP level. These devices offer more stable pressure during expiration but require the user to overcome the load, which can retard expiratory flow, particularly at rest and during the early phases of exercise. In contrast, flow-dependent PEP devices generate PEP by breathing through a small orifice. While the pressure delivered may vary with the subject’s expiratory flow rate, these devices do not interrupt the expiratory flow.
Conical-PEP is a flow-dependent PEP device, where varying diameters of orifices act as resistors to generate PEP. Our previous study used conical-PEP resistors made from plastic sheets and applied with an oronasal mask. However, this setup occasionally led to unstable attachment during application. Furthermore, only a limited range of resistors (sizes 5 mm, 6 mm, and 7 mm) was developed and used in the previous study.11 Based on our experience, the 7 mm orifice was not large enough to provide sufficient PEP for some subjects with a high expiratory flow rate during exercise. Moreover, the conical-PEP resistor was selected to achieve a peak expiratory pressure of 5 cmH₂O based on the expected expiratory flow rate during exercise.11
However, we acknowledge that a target pressure of 5 cmH₂O may not be suitable for all COPD patients due to variations in pathology and dynamic hyperinflation. Therefore, we hypothesized that a formula to calculate the minimum required PEP may help individualize the selection of an appropriate conical-PEP resistor. Moreover, we modified the conical PEP using more durable materials through 3D printing and expanded the range of resistors to nine sizes (4 mm, 4.5 mm, 5 mm, 5.5 mm, 6 mm, 6.5 mm, 7 mm, 7.5 mm, and 8 mm).12 Our aim is to investigate the effect of conical-PEP with minimal required PEP level on exercise duration, DH, and dyspnea in patients with moderate to severe COPD.
Methods
Study design and setting
This study was a single-blind, randomized crossover design (with blinded subjects) conducted in COPD patients. Participants were recruited between September 2021 and May 2023 from Srinagarind Hospital, Nam Phong Hospital, and Phra Yuen Hospital in Thailand. The study was conducted in the research room of the Faculty of Associated Medical Sciences, Khon Kaen University. The study was approved by the Khon Kaen University Ethics Committee in Human Research (HE641234, approved date 10 Aug 2021) and registered with the Thai Clinical Trial Registry (TCTR20230124006). Informed consent was obtained from all subjects before commencing the study.
Subject eligibility
Inclusion criteria included COPD with GOLD stage II to IV, aged between 49 and 80 years, with a diagnosis of COPD (FEV1/FVC < 0.7), good cooperation, cognitive and communication skills (assessed using the Mini-Mental State Examination with a cutoff score of 26),13 and no exacerbations within the previous four weeks. Subjects were excluded if they had any contraindications to exercise testing according to the European Respiratory Society’s statement on the standardization of cardiopulmonary exercise testing in chronic lung diseases, such as uncontrolled cardiovascular conditions, uncontrolled respiratory conditions, uncontrolled non-cardiorespiratory conditions affecting or aggravated by exercise, advanced or complicated pregnancy, resting oxygen saturation (SpO2) ≤85% on room air, or musculoskeletal problem that compromises exercise performance.14
Conical PEP and resistor size selection procedure
The type of PEP device used in this study was conical-PEP, a flow-dependent PEP with a cone-shaped design. It has an inlet orifice measuring 13.0 mm in diameter and an outlet orifice with eight different resistor sizes: 4.5, 5.0, 5.5, 6.0, 6.5, 7.0, 7.5, and 8.0 mm. These outlet sizes serve as airflow resistors. The total length of the cone is 10 mm (see Figure 1A). The conical PEP device was integrated with a non-rebreathing oronasal mask, as illustrated in Figure 1B.
The following procedure was used to determine the appropriate conical-PEP resistor size for each subject:
1. Incremental Spot Marching Test (ISMT)
Procedure: The Incremental Spot Marching Test (ISMT) was used to determine peak exercise capacity by progressively increasing the intensity of the exercise. This test involved three phases: resting 5 mins (in relaxed sitting position), exercise phase (performing spot marching) and recovery at least 5 mins (in relaxed sitting position). Incremental spot marching consists of marching in place, alternating between knee raises (hip flexion 45-70 degrees) and arm raises above shoulder height (shoulder flexion at least 90 degrees). Thus, increasing the stepping rate led to an increase in exercise intensity.3,11 The test began at a stepping rate of 70 steps per minute, with increments of 10 steps per minute every 3 minutes. Stepping rates were controlled using a metronome. Visual feedback was provided to ensure the target range of motion by marking the individualized height of the arm and leg raises on the wall in front of the participants using coloured tape. Additionally, verbal feedback was given to encourage consistent step rates and range of motion.3 The participants continued the test until they met the termination criteria of the test. Peak stepping rates, the duration of the exercise, and the reason for termination were recorded.
Prior to the ISMT, all subjects were instructed as follows: rest for at least two hours before testing, refrain from performing strenuous activity for at least 24 hours, avoid caffeine on the day of the test, and refrain from smoking for at least eight hours.14 Moreover, subjects were advised to use their usual inhalers at least 20 minutes before the doctor-prescribed exercise test.
Termination criteria: The termination criteria were if subjects had signs or symptoms to terminate exercise, uncoordinated step rate, or met some termination criteria. These criteria include participants’ desire to stop exercise, rating perceived of breathlessness by Borg CR 10 (RPB) ≥ 7 or rating perceived of exertion by Borg CR 10 (RPE) ≥ 8, SpO2 < 88% at room air,15 or the subjects want to stop. A deviation in the stepping rate of ±5% was acceptable, but if the uncoordinated rate exceeded ±5% and verbal cues could not correct it, the test was terminated.3
Flow and pressure measurement during ISMT: During the ISMT, the subjects wore an oronasal facemask (V2TM Mask, HANS RUDOLPH, Inc., USA) connected to the SS11LA transducer, which measured the flow rate, and the SS19L transducer, which measured expiratory pressure. Both transducers were connected to the Biopac MP36 system. Peak expiratory mouth pressure at rest, peak expiratory mouth pressure at the end of exercise, and end-exercise expiratory flow rate were assessed.
Safety and physiological response monitoring: Heart rate (HR), electrocardiograph (ECG), SpO2, respiratory rate (RR), and end-tidal carbon dioxide (PetCO2), was performed every minute during resting conditions (at least 5 minutes), the ISMT, and recovery conditions (at least 5 minutes). Blood pressure (BP) was monitored every two minutes during resting and recovery conditions. RPB and RPE were also recorded every minute using the modified Borg scale during rest, ISMT, and recovery. Expiratory mouth pressure was measured and monitored throughout the exercise phase.
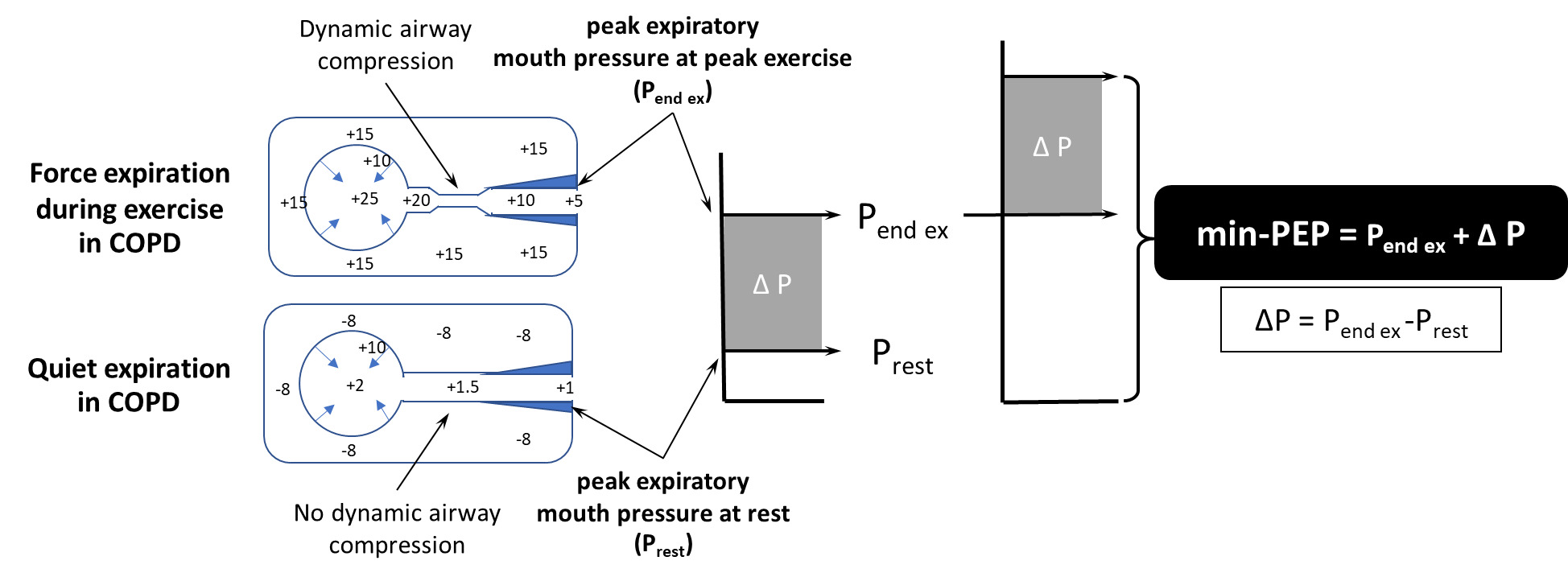
2. Minimum PEP level requirement
The minimal PEP (min-PEP) required was estimated using the following hypothesis. The end exercise pressure is thought to be insufficient to prevent dynamic airway compression in patients with COPD.9,16,17 Therefore, additional pressure or PEP above this end exercise pressure is required to counteract the dynamic airway compression.11,18–23 Moreover, the resting pressure is a baseline pressure that should not be ignored. Therefore, the minimum PEP requirement was hypothesized using the following equation.
min-PEP=Pend-ex +(Pend-ex−Prest)
= minimum level of positive expiratory pressure
= Peak mouth expiratory pressure in resting condition
= Peak mouth expiratory pressure in end-exercise condition
(Note: The pressures were measured during the ISMT) (see Figure 2).
3. Selection of the Conical PEP resistor size
The largest orifice that provided min-PEP consistent with the end-exercise expiratory flow rate during the ISMT was selected. The selected orifice was then tested on subjects by simulating forced expiration, similar to that during exercise, to ensure comfort and confirm that the maximum pressure did not exceed 35 cmH₂O.24
Intervention
The effect of the conical PEP with mini-PEP level (conical-PEP) was tested using the Endurance Spot Marching Test (ESMT).11 The procedure for the ESMT was similar to that of the ISMT, with the key difference being the use of the peak step rate achieved during the ISMT as a constant load.
A selected conical-PEP resistor was integrated into a non-rebreathing oronasal facemask (3M 6000 series), which was worn during the last minute of the resting phase and throughout the ESMT. The subjects breathe in through a one-way valve and breathe out through conical-PEP resistors. The subjects performed the ESMT until they met the termination criteria described above in the ISMT. The duration of the exercise test and the reason for termination were recorded. A washout period of at least 30 minutes was provided, ensuring that subjects’ vital signs returned to resting conditions. The termination criteria, safety measures, and physiological response monitoring for the ESMT were consistent with those used in the ISMT.
A previous study on the use of the conical-PEP device reported no adverse events in patients with chronic obstructive pulmonary disease.11 However, potential discomforts such as dizziness, severe breathlessness, or barotrauma (commonly referred to as “airplane ear”) were considered as precautions in the present study. If these events occurred, the study protocol included plans for immediate termination of the exercise.
Sham-PEP
The subjects performed the ESMT while wearing the same non-rebreathing oronasal facemask (3M 6000 series) without a conical-PEP resistor incorporated (subject blind). The mask was worn during the last minute of the resting phase and throughout the ESMT. The subjects performed the ESMT until they met the termination criteria described above in the ISMT. The duration of the exercise test and the reason for termination were recorded. A washout period of at least 30 minutes was provided, ensuring that subjects’ vital signs returned to resting conditions. The termination criteria, safety measures, and physiological response monitoring for the ESMT were consistent with those used in the ISMT.
Outcome measurements
-
Demographic Data: After obtaining informed consent, demographic data, including age, gender, comorbidities, and usual medications, were recorded from the participant’s medical records during their chest-clinic appointment. Height and weight, measured by clinical staff on the same day, were also recorded from the medical records. The Modified Medical Research Council (mMRC) Dyspnea Scale was also administered prior to the start of the study.
-
Endurance Time/Exercise Time: The primary outcome is the ESMT’s exercise time, representing exercise capacity.
-
Dynamic Hyperinflation (DH): DH was determined by measuring the decrease in IC (Puente-Maestu and Stringer, 2006). IC was measured three times before and immediately after the ESMT (within 30 seconds) using a Biopac MP36 device, which converts inspiratory flow rate and time into volume. The average of 3 times was reported.
-
Dyspnea: Dyspnea was assessed using the rating of perceived breathlessness by Borg CR10, which ranges from 0 to 10 during resting and exercise.25
-
Exertion: Exertion was assessed using the rating of perceived exertion by the modified Borg scale, which ranges from 0 to 10 during resting and exercise.25
Sample size determination
No previous studies have investigated the effect of mini-PEP using conical-PEP on exercise endurance time in patients with COPD, making it challenging to calculate the sample size. Therefore, a pilot study was conducted with 10 patients with moderate to severe COPD. The pilot study data revealed a mean endurance time of 4.20±1.97 minutes in the sham-PEP condition and 4.82±1.94 minutes in the conical-PEP condition, yielding an effect size of 0.653. Using G*Power (v 3.1.9.7) for a paired, two-tailed t-test to compare means, it was estimated that a sample size of 21 subjects would be required to detect a statistically significant difference with 80% power at 𝛼 = 0.05.
Randomization
Block randomization was performed by N.K. to assign participants to either the sham-PEP followed by conical-PEP or conical-PEP followed by the sham-PEP, with a 1:1 allocation ratio. The randomization process used two blocks of size six and one block of size four. Each sequence was placed in a sealed envelope. N.K. enrolled the participants, and A.A.N. assigned them according to the sequences in the sealed envelopes.
Statistical analysis
Descriptive statistics were reported as mean ± SD or median with IQR. The data distribution was assessed using the Shapiro-Wilk test/Stem and leaf plot. Depending on the data distribution, the Wilcoxon signed-rank test or the paired t-test was used for analysis. Statistical significance was considered when p < 0.05. SPSS version 27 was used to analyze all data. Heart rate maximum (HRmax) was calculated using the following equation: HRmax = 206.9-(0.69 x age in years).26 Percent heart rate reserve was calculated by the Karvonen method. Iso-time extracted the shortest exercise time in control or conical-PEP conditions in each subject.
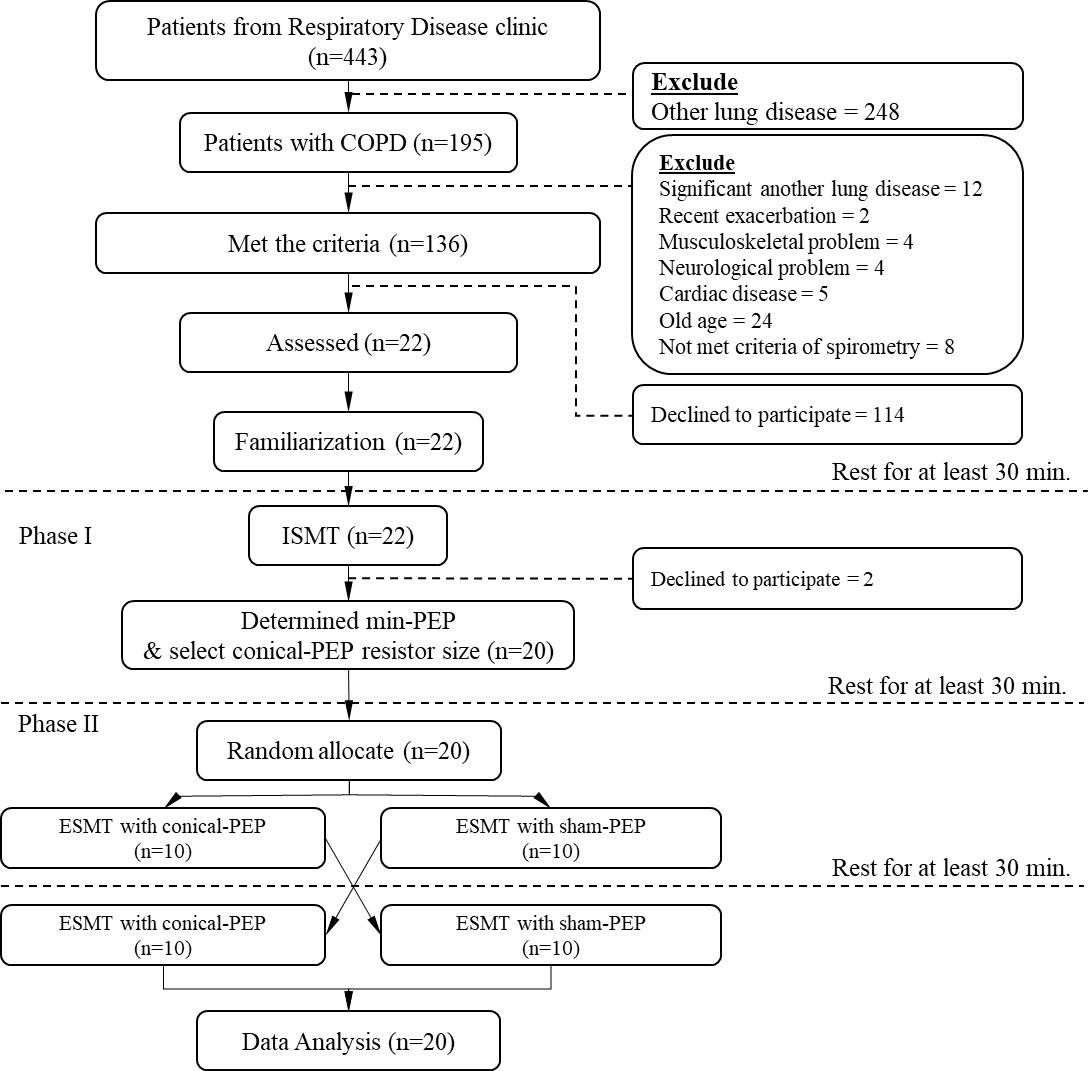
Results
Twenty-two subjects with COPD were enrolled between September 2021 and May 2023. Two subjects dropped out because they wanted to withdraw from the study after the ISMT. Therefore, 20 subjects completed the study (see Figure 3). Demographic characteristics of the subjects are shown in Table 1.
ISMT response
The peak step rates of ISMT were 70 steps/min (n = 12), 80 steps/min (n = 4), 90 steps/min (n = 2), and 100 steps/min (n = 2). Median exercise time around 2.92 [1.59, 5.83] min. The participants’ exercise intensity was moderate, 71±11% of age-related maximum heart rate. All the participants stopped ISMT mainly due to dyspnea and exertion, with a median (IQR) of RPB 5 [5,6] and RPE 4 [3, 5]. The peak expiratory flow rate at resting and end of the exercise was reported as 0.62±0.17 and 1.59±0.50 L/s. The expiratory pressure was a median of 0.86 [0.54, 1.06] cmH2O and 3.17 [2.34, 4.51] cmH2O at resting and end exercise, respectively. Exercise responses of ISMT are shown in Supplement 1. The calculated mini-PEP was a median of 5.46 [3.84, 8.61] cmH2O, and the conical-PEP resistor sizes were 8 mm (n = 19) and 7.5 mm (n = 1). HR, EKG, SpO2, RR, BP and End-tidal CO2 were within the safety zone during and recovery phases of ISMT (see Supplement 1).
Effect of conical-PEP on exercise time
Table 2 shows the ESMT responses for conical-PEP and sham-PEP conditions. ESMT endurance time was significantly longer in the conical-PEP condition (4.98 ± 2.97 minutes) compared to the sham-PEP condition (3.99 ± 2.19 minutes) (∆=1.07 min, 95% CI 0.39 to 1.74 min, p = 0.004) (see Figure 4).
Effect of conical-PEP on dynamic hyperinflation
IC showed no significant difference between the two conditions at rest (sham-PEP: 1.51 L [1.32, 2.19]; conical-PEP: 1.58 L [1.33, 2.11]; p = 0.344). Both conditions showed a significant decrease in IC at the end of exercise compared to baseline (p = 0.007 for sham-PEP and p = 0.036 for conical-PEP). However, IC at the end of exercise was significantly greater in the conical-PEP condition (1.51 [1.24, 1.85] L) compared to the sham-PEP (1.42 [1.16, 1.84] L) (p = 0.020) (see Figure 5).
Figure 5. (A) IC response to exercise in conical-PEP and control conditions, (B) Individual’s IC response in conical-PEP condition, (C) Individual’s IC response in sham-PEP condition, (D) Distribution of IC change in conical-PEP condition, (E) Distribution of IC change in sham-PEP condition.
Note. IC data of one subject was not available in both conditions due to equipment error and is shown in median (Q1, Q3). Exercise time mean +/-SD. * p = 0.020 between conical-PEP and sham-PEP conditions at end exercise IC by Wilcoxon signed rank test.
Effect of conical-PEP on dyspnea
At the end of the exercise, RPB did not differ significantly (median score of 5 in both conditions). However, at iso-time (3.82 ± 2.09 min), conical-PEP showed a significantly lower median RPB (4 [4, 5]) compared to sham-PEP (5 [5, 6]) (p = 0.005) (see Figure 6).
Physiologic and perceptual responses of conical-PEP and sham-PEP conditions during ESMT
The physiological and perceptual responses during ESMT of both conditions are shown in Table 3. HR, EKG, SpO2, RR, BP and End-tidal CO2 were within the safety zone during and recovery phases of ESMT in both conical-PEP and sham-PEP conditions. Resting expiratory pressure was 0.15 [0.12, 0.16] cmH2O in the sham-PEP and 1.02 [0.94, 1.18] cmH2O in the conical-PEP conditions. At the end of ESMT, the median peak expiratory pressure was 0.25 [0.22, 0.28] cmH₂O in the sham-PEP and 4.39 [3.31, 7.38] cmH₂O in the conical-PEP conditions (p < 0.001). The calculated min-PEP from our formula was 5.46 [3.84, 8.61] cmH₂O. The median difference between calculated min-PEP and actual delivered peak PEP was -0.004 [-0.973, 1.706] cmH₂O (see Table 2).
Discussion
PEP has been a prominent focus in COPD research over the past 15 years, particularly for its role in improving exercise capacity by delaying or preventing the development of DH. However, evidence on the effects of conical-PEP in COPD, particularly regarding exercise capacity and DH, remains limited. Therefore, we investigated the effects of conical-PEP on exercise capacity, DH, and dyspnea in patients with moderate to severe COPD. Our findings indicate that the application of conical-PEP during exercise enhances exercise capacity, as measured by exercise time, while delaying the onset of dyspnea and DH.
The HR response at the end of exercise was around 116 bpm in both the conical-PEP and sham-PEP conditions, corresponding to 72% of maximum heart rate. This indicates that the exercise intensity was moderate to high in both conditions. Therefore, since the exercise intensity was comparable between the two conditions, the results regarding exercise capacity are likely to be comparable as well.
Our study found that exercise endurance time was significantly improved with conical-PEP, showing a median increase of 25.94% [11.43, 44.33] compared to the sham-PEP group. However, two subjects exhibited reduced exercise time with conical-PEP, although no specific reason was identified (see Figure 4). Furthermore, IC measured immediately at the end of exercise was significantly better in the conical-PEP condition compared to the control condition (see Figure 5), suggesting that incorporating conical-PEP during exercise in patients with COPD delays the development of DH. There was no significant difference in dyspnea between the two conditions at the end of exercise, which is expected since dyspnea commonly determines the point of exercise termination. However, at iso-time (3.82 ± 2.09 minutes), dyspnea was significantly lower in the conical-PEP condition, suggesting a delayed development of symptoms, likely due to the reduced onset of DH. This improvement in dyspnea is consistent with the significant increase in IC, indicating reduced DH in the conical-PEP condition compared to the control. In the recovery phase, a similar dyspnea response was observed between the conical-PEP and sham-PEP conditions, likely because the masks were removed immediately after exercise, allowing recovery without the continued influence of PEP, resulting in a comparable response between the two conditions.
Few studies have reported the effects of conical-PEP on exercise capacity, DH, and dyspnea in patients with COPD. Therefore, the comparison of our findings with those of previous studies is limited. The effects of conical-PEP during exercise were reported by Ubolsakka-Jones et al. in patients with moderate to severe COPD, where they applied conical-PEP resistors with 5-, 6-, or 7-mm orifices (median peak expiratory pressures of 4.5 [3.2–6.2] cm H2O at the end of exercise). They found that exercise capacity, as measured by endurance exercise time, was significantly improved compared to the control condition. However, their study showed no significant difference in DH by immediate post-exercise IC between the conical-PEP and control conditions.11 Similarly, while there was no significant difference in dyspnea at the end of exercise, it was significantly reduced at iso-time in the conical-PEP condition compared to the control in their study.
Therefore, our findings of improved exercise capacity and delayed onset of dyspnea are consistent with the previous study by Ubolsakka-Jones et al.11 However, while our study demonstrated a significant improvement in DH compared to the sham condition, the previous study did not observe significant changes in DH when comparing conical-PEP to the control condition. This inconsistency may be attributed to the more defined protocol for conical-PEP resistor selection in our study. Ubolsakka-Jones et al. reported that the conical-PEP resistor was selected based on expected expiratory flow,11 whereas in our study, the resistor was chosen based on individualized mini-PEP, which was estimated according to our hypothesis equation, considering each subject’s expiratory flow rate and pressure.
On the other hand, Wibmer et al. found that incorporating flow-dependent PEP with a fixed 5mm orifice (PEP around 10-20 cmH2O) during exercise via a nasal mask significantly reduced exercise capacity, as measured by a 6-minute walk distance, compared to the control group in patients with COPD.27 Despite using a similar flow-dependent PEP, Wibmer et al. reported inconsistent findings. In our study, we used a non-rebreathing oronasal mask that allowed participants to breathe through both the mouth and nose. The greater flexibility in breathing allowed in our study may help explain the contrasting findings in exercise capacity compared to the previous study by Wibmer et al.
Furthermore, Bhatt et al. reported an improvement in the 6MWD with pursed-lip breathing (PLB) compared to normal breathing.18 Faager et al. also reported that PLB improved the endurance shuttle walk test compared to the control.28 These finding support the use of PLB that generates back pressure, similar to flow-dependent PEP devices, to enhance exercise performance.
There was no difference in RR, HR, and BP between the estimated PEP and control in our study. A previous study by Ubolsakka-Jones et al. found that RR was slower in the conical PEP group compared to the control, although HR and BP were not different between the two conditions.11 Our study did not instruct the participants to modify their breathing patterns with PEP, which may explain why the RR was not slower than in the control group.
The calculated min-PEP from our formula was 5.46 [3.84, 8.61] cmH₂O, while the conical-PEP device generated a median peak PEP of 4.39 [3.31, 7.38] cmH₂O. The median difference between the two values was -0.004 [-0.973, 1.706] cmH₂O. This slight difference may be attributed to the flow-dependent nature of the conical-PEP device, as variations in flow can cause the delivered PEP to differ from the calculated PEP. On the other hand, the threshold PEP device can provide a more precise calculated PEP. However, it has certain limitations, such as the absence of expiratory flow at the start of exhalation until sufficient pressure builds to open the threshold, and the need to maintain this pressure throughout the entire exhalation. These factors can make forced exhalation more challenging at rest and during exercise, particularly when the drive to breathe increases, potentially resulting in discomfort.
Our study confirms the benefit of conical-PEP in improving exercise duration, reducing the development of DH, and improving dyspnea using a resistor selected based on the min-PEP level in a single session. An 8 mm resistor was used in all participants except one, who required a 7.5 mm orifice. Participants were continuously monitored for heart rate, blood pressure, SpO₂, PetCO2, and ECG during both exercise and recovery, with no adverse events or patient-reported issues observed. The peak PEP delivered ranged from 2 to 11 cmH₂O at the end of exercise, remaining well below the 35 cmH₂O. Therefore, in clinical settings where flow and pressure cannot be measured, starting with an 8 mm resistor under supervision, followed by stepwise titration to smaller sizes (e.g., 7.5 mm or 7 mm) based on clinical response, may be a practical approach. Similar monitoring is recommended during the familiarization phase or initial exercise session to ensure patient safety.
In this study, the majority of participants were male (19 out of 20; 95%). One contributing factor was the exclusion of four female COPD patients due to severe knee osteoarthritis (musculoskeletal problem), which prevented participation. Therefore, the findings should be interpreted with caution, as they may not be generalizable to both genders.
Our study has some limitations. Firstly, we used the conical-PEP device, so our results may not be generalizable to all PEP devices used in COPD treatment. Additionally, our findings cannot be directly compared with those from studies using other types of PEP devices. We were unable to measure IC at iso-time, which might have demonstrated clearer differences in dynamic hyperinflation between the two interventions. However, obtaining IC at the exact iso-time point is impractical, as repeated measurements during exercise interfere with breathing mechanics. The min-PEP calculation was based solely on our theoretical knowledge and hypothesis. However, it is limited in its ability to measure the extent of dynamic airway compression during exercise in our setting, and therefore, it was not possible to determine the mini-PEP required to counteract this compression. In addition, this crossover study compared conical-PEP at the minimum effective level with a sham-PEP condition, with at least a 30-minute washout between the two interventions conducted on the same day. The aim was to examine the immediate effects of conical-PEP on exercise duration, DH, and dyspnea in a single exercise session. Therefore, follow-up was not feasible in this design. Future research should focus on optimizing the calculation of the minimum effective PEP using evidence-based formulas, including a larger sample size, and evaluating the long-term effects of conical-PEP within pulmonary rehabilitation programs, with particular emphasis on clinically relevant outcomes such as quality of life.
Conclusion
The use of conical-PEP device with a resistor selected to achieve the minimum required PEP level during exercise in COPD patients improved exercise endurance, delayed the development of DH, and delayed the onset of dyspnea.
Acknowledgement and funding
We would like to express our sincere gratitude to the participants of this study for their valuable contributions. We also extend our appreciation to the medical professionals and experts (Dr.Benjarat Sangthong, Assoc. Prof.Dr.Wantana Siritaratiwat and, Dr.Saowanee Nakmaroeng) who generously shared their knowledge and insights. We appreciate the funding support from the Postdoctoral Training Type 1 Grant from the Faculty of Associated Medical Sciences, Khon Kaen University. This work (Grant No. RGNS 65-048) was supported by the Office of the Permanent Secretary, Ministry of Higher Education, Science, Research and Innovation (OPS MHESI), Thailand Science Research and Innovation (TSRI), and Khon Kaen University.
Conflicts of interest
The authors have completed the ICMJE forms and declare no conflicts of interest.
Ethical Approval
The study was approved by the Khon Kaen University Ethics Committee in Human Research (HE641234, approved date 10 Aug 2021) and registered with the Thai Clinical Trial Registry (TCTR20230124006).
Declaration of Generative AI and AI-Assisted Technologies in the Writing Process
During the preparation of this manuscript, the authors used ChatGPT solely to improve the clarity of English writing. Subsequent to utilizing this tool, we reviewed and revised the content, taking full responsibility for the publication’s material.

_conical-pe.png)

_spot_marching_endurance_time_(data_presented_as_mean__sd)__(b)_individual_spot_ma.png)
_ic_response_to_exercise_in_conical-pep_and_control_conditions__(b)_individual_s_ic_res.jpeg)
_and_recovery_(b)_conical-pep_and_.png)
_conical-pe.png)
_spot_marching_endurance_time_(data_presented_as_mean__sd)__(b)_individual_spot_ma.png)
_ic_response_to_exercise_in_conical-pep_and_control_conditions__(b)_individual_s_ic_res.jpeg)
_and_recovery_(b)_conical-pep_and_.png)