Introduction
Intraoperative air leakage from the endotracheal tube (ETT) cuff can lead to catastrophic complications due to inadequate minute ventilation and an increased risk of aspiration. The severity of these complications depends on the degree of leakage and, in extreme cases, can result in complete ventilatory failure. This may lead to aspiration, hypoxia, hypercarbia, and even cardiac arrest. The incidence of intraoperative air leaks around the ETT cuff ranges from 5.9% to 11%.1
Although a structural defect in the ETT cuff or pilot balloon system is often suspected as the primary cause of intraoperative air leaks, several other factors may contribute, including cephalad migration of the ETT, displacement of orogastric or nasogastric tubes into the trachea, underinflation of the ETT cuff, and inappropriate ETT size.1 Prompt identification of the underlying cause is crucial for determining the appropriate intervention to minimize airway-related complications and prevent disruptions to the surgical procedure. Immediate management is warranted in such situations.
The definitive management of intraoperative ETT air leaks is replacing the ETT when other corrective measures fail. However, this can be challenging, especially in surgical positions where the patient is not supine, such as prone or lateral positions.2 In neurosurgical procedures, an additional challenge arises from the proximity of the surgical field to the airway. Once surgery has commenced, concerns about contaminating the sterile field further complicate airway interventions. Therefore, meticulously confirming ventilatory status and checking all connections in the breathing circuit before the final surgical positioning is of paramount importance.
Over the past few decades, significant advancements in ETT design have reduced the risk of aspiration and airway-related complications.3 With the availability of modern equipment and monitors, these complications can be identified early and managed appropriately.
In this report, we describe a case of intraoperative endotracheal cuff leakage detected after the initiation of the surgery in the prone position. We innovatively managed this challenge using an ETT cuff manometer, successfully preventing airway-related complications.
Findings
A 28-year-old male diagnosed with a left parietal high-grade glioma was scheduled for craniotomy and tumour excision in the prone position. After induction of general anesthesia with intravenous fentanyl (2 mcg/kg), propofol (2 mg/kg), and rocuronium (0.5 mg/kg), an 8.5 mm cuffed flexometallic endotracheal tube (ETT) was placed via direct laryngoscopy and secured at 22 cm. A flexometallic ETT was preferred due to its wire reinforcement, providing kink resistance and easier angulation. Significant neck flexion was required for optimal surgical exposure, further justifying the choice of a flexometallic ETT over a polyvinyl chloride (PVC) ETT.
Prior to insertion, the ETT cuff was inflated and visually checked for any air leakage. After placement, end-tidal CO₂ tracing was confirmed via capnography, and the ETT cuff was inflated to a pressure of 25 cm H₂O. Bilateral air entry was verified by auscultation, and mechanical ventilation was initiated without any air leak at that point. Bilateral air entry was reconfirmed after positioning the patient in the prone position. General anesthesia was maintained with an air-oxygen mixture (1:1) along with sevoflurane, targeting a minimum alveolar concentration (MAC) of 0.8-1. Intravenous fentanyl and rocuronium infusions were also administered. Mechanical ventilation was set to Volume-Controlled Mode with the following parameters: tidal volume - 450 mL, respiratory rate - 12/min, and positive end-expiratory pressure (PEEP) - 5 cm H₂O.
One hour into surgery, the ventilator alarm indicated a fresh gas flow leak and failure to deliver the set tidal volume, with a detected leak of 200-300 mL per cycle. Increasing the tidal volume did not resolve the issue (Figure 1). Since the problem was addressed immediately, the patient remained hemodynamically stable with no desaturation. Examination of the ETT revealed a deflated pilot balloon. Manual inflation with a syringe temporarily reduced the leak and restored adequate ventilation. However, the issue recurred after 10 minutes, raising suspicion of ETT cuff malfunction.
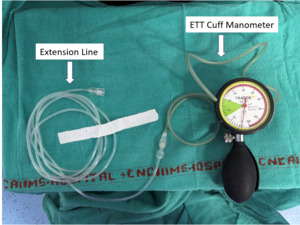
To facilitate intraoperative management, the pilot balloon was connected to a 2-meter extension line, with the distal end attached to a cuff pressure manometer (Tracoe Cuff Pressure Monitor Sensitive, Atos Medical, UK) (Figure 2). This setup enabled continuous monitoring of ETT cuff pressure and allowed for repeated inflation whenever the pressure dropped below 20 cm H₂O or a fresh gas flow leak was detected. This innovative approach provided quantitative cuff pressure assessment and ensured adequate intraoperative ventilation. As the ventilatory leak decreased, replacing the ETT intraoperatively was deemed unnecessary. Throughout the nine-hour surgery, adequate minute ventilation was maintained with stable hemodynamic parameters and arterial blood gas values. No episodes of desaturation or hypoxia occurred.
At the end of surgery, the flexometallic ETT was removed and examined using methylene blue dye to detect any leak in case of cuff or pilot balloon rupture. The test revealed a malfunction of the one-way inflation valve in the pilot balloon, leading to gradual cuff deflation.
Discussion
Leaks following endotracheal tube (ETT) placement can arise from multiple causes.1 ETT cuff leaks can be broadly classified into two categories: those due to defects in the cuff and/or inflation system and those due to leaks around an intact cuff. Air leaks around an intact cuff may result from cuff underinflation, inappropriate ETT size, cephalad migration of the tube into the supraglottic region, or misplacement of a nasogastric or orogastric tube into the trachea.4–6 Leaks due to structural defects in the cuff or inflation system may occur due to a damaged cuff, a punctured pilot balloon or inflation line, or a defective one-way inflation valve.7,8
Intraoperative ETT air leaks can be harmful to both the patient and the operating room personnel. During surgery, these leaks may lead to serious complications such as aspiration and inadequate minute ventilation.9 Additionally, they can interfere with the delivery of anesthetic gases when inhalational agents are used to maintain general anesthesia, potentially resulting in inadequate anesthetic depth. This, in turn, increases the risk of intraoperative awareness and its associated consequences. In neurosurgical patients, insufficient anesthesia can elevate intracranial pressure and trigger coughing, straining, and patient movement, all of which can negatively impact surgical outcomes. Furthermore, leakage of inhalational anesthetic agents contributes to operating room pollution, exposing the personnel to their effects.10,11
Several techniques have been described in the literature for managing intraoperative ETT air leaks. The first step in management is identifying the cause of the leak. The integrity of the cuff and inflation system can be assessed using a manometer to measure intracuff pressure, which helps determine whether the cuff is underinflated.12 If a manometer is unavailable, other techniques can be used, such as manually palpating the pilot balloon or adjusting the cuff volume while monitoring the ventilator for air leaks. Although continuous intracuff pressure monitoring is not routinely performed, periodic checks can aid in the early detection of leaks.13
Identifying leaks due to structural defects in the intraoperative period can be challenging, as all components of the ETT cannot be separately assessed. Pre-insertion integrity checks of the ETT cuff and inflation system are standard practice to identify defects and prevent airway-related complications. However, these inspections must be performed aseptically to minimize contamination risk.14 Visual inspection of the cuff and pilot balloon alone may not detect minimal leaks. Submersion of the ETT in water to identify air bubbles has been described as a method for detecting small leaks,15 though its routine use in clinical practice is limited. In our case, the pre-insertion check did not reveal an air leak, as the defect was minor and resulted in a slow, progressive cuff deflation.
Various strategies have been described for managing intraoperative ETT cuff leaks. The choice of intervention depends on factors such as surgical duration, the degree of leak, adequacy of ventilation, and patient positioning. The definitive management is ETT replacement, but this is not always feasible intraoperatively and should be considered a last resort. Temporary measures to reduce air leaks include pharyngeal packing, injection of lignocaine jelly into the pilot balloon, and continuous inflation of the pilot balloon. Pharyngeal packing can reduce leaks to some extent but does not eliminate micro-aspiration risk. Additionally, it is difficult to perform once the patient is in the prone position or after surgery has commenced.2
Leaks in the inflation system have been previously managed by cutting the inflation line distal to the site of the defect and inserting a 22-gauge intravenous cannula, which is then attached to a clave, allowing for air reinflation as needed.16,17 In cases where the one-way inflation valve is incompetent, sealing it with a three-way stopcock can prevent air loss while enabling reinflation when necessary. For cuff leaks, continuous inflation using an oxygen flowmeter attached to the inflation line has been used to maintain cuff volume and prevent leaks.18 A similar method was previously employed during cerebral aneurysm surgery, where an infusion pump delivered a constant volume of air to the cuff to maintain pressure, thereby preventing deflation and leakage.19
Alternatively, a commercially available pilot tube repair kit can be used to manage intraoperative ETT leaks by sealing a defective inflation valve or pilot balloon. However, this device was not available at our institution and could not be used in our case. If a faulty pilot tube is found to be the reason for the leak, the pilot tube is cut below the damaged part. These kits can then be inserted into the cut pilot tube, and in the usual manner, the cuff can be re-inflated. However, if the cuff is damaged, these kits cannot improve air leaks.20 When conservative measures fail, ETT exchange remains the only option. Anaesthesiologists must carefully assess the risk-benefit ratio of exchanging the ETT in the prone position versus repositioning the patient supine. Changing position intraoperatively can be extremely challenging without breaching the sterility of the surgical field, disrupting the procedure, or, in critical moments such as controlling major bleeding, leading to catastrophic consequences. Therefore, ETT exchange in the prone position should only be performed by an experienced anaesthesiologist with thorough preparation, including ready access to equipment for managing accidental extubation and difficult airways.
Due to limited airway access, accidental extubation in the prone position is particularly difficult to manage. According to an algorithm from the existing literature, immediate assistance from operating room personnel is crucial in such situations. A second-generation supraglottic airway device can be used to rapidly secure the airway and restore mechanical ventilation. If adequate ventilation is achieved and surgery can continue without significant complications, the supraglottic airway may be retained. However, if there is an increased aspiration risk or inadequate ventilation, fiberoptic intubation through the supraglottic device may be attempted. If all measures fail, the patient should be promptly repositioned to supine, and the airway secured without delay.21,22
A video laryngoscope can be invaluable during a planned ETT replacement, especially when in prone position. However, manoeuvring a video laryngoscope in this position presents challenges and requires expertise to minimize re-intubation time. The blade should be inserted similarly to an oropharyngeal airway, considering the patient’s downward-facing position. A channelled-blade video laryngoscope has been found to facilitate reintubation in the prone position more effectively.23,24 Additionally, inserting an airway exchange catheter (AEC) or bougie into the existing ETT before removal allows the new tube to be railroaded over it, reducing the risk of failed intubation. The AEC also provides temporary oxygenation if re-intubation is prolonged. Among supraglottic devices, studies have shown that the I-gel provides easier insertion compared to the Classic Laryngeal Mask Airway (LMA) and ProSeal LMA.25
In our case, the ETT leak was attributed to a malfunction of either the cuff or the pilot balloon and inflation system. Connecting the pilot balloon to a 2-meter extension line attached to a cuff pressure manometer not only allowed for repeated inflation but also enabled continuous monitoring of cuff pressure, facilitating early detection of even minor leaks. This approach also prevented manual overinflation, which can cause tracheal mucosal injury and increase the risk of postoperative sore throat. Although various techniques have been described for managing similar airway complications, none have incorporated continuous ETT cuff pressure monitoring using a manometer. This method provides real-time quantitative assessment and management of ETT leaks. While multiple management strategies exist, literature on addressing such complications in the prone position remains scarce. Prompt, innovative thinking and skilled management are crucial for ensuring patient safety and surgical success in these situations.
Conclusion
The innovative use of the ETT cuff manometer not only aids in managing air leaks but also enables continuous, quantitative monitoring of cuff pressure, facilitating early leak detection. This approach underscores the importance of swift emergency management using available resources, thereby preventing complications and improving patient outcomes.
Funding
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing interests
All authors have completed the ICMJE uniform disclosure form and declare no conflict of interest.
Ethical approval
Not required for this article type. Informed consent was obtained from the patient.
AI Statement
The authors confirm no generative AI or AI-assisted technology was used to generate content.

_ventilator_alarm_indicating_fresh_gas_flow_leak__b)_cuff_manometer_showing_low_cuff_pre.png)
_ventilator_alarm_indicating_fresh_gas_flow_leak__b)_cuff_manometer_showing_low_cuff_pre.png)
