Introduction
An increase in respiratory work can lead to respiratory muscle fatigue, which results in the activation of type III and IV afferent fibres, primarily from the diaphragm muscle.1–3 This activation is associated with peripheral vasoconstriction, an increase in mean arterial pressure (MAP), heart rate (HR) and redirection of blood flow from skeletal to respiratory muscles, which may result in reduced exercise capacity.4–6 This phenomenon is known as inspiratory muscle metaboreflex (IMM).
The IMM can occur in healthy persons and those with diseases such as chronic obstructive pulmonary disease (COPD) and heart failure.7–9 Studies have demonstrated that a reduction in the activity of type III and IV afferent fibres can attenuate the IMM and increase exercise capacity.4,5 For example, one study with COPD patients reported that using assisted ventilation to decrease respiratory load during high-intensity exercise increased blood flow to skeletal muscle and exercise tolerance time (Tlim).10 Inspiratory muscle training (IMT) is an intervention used in healthy individuals and those with various diseases, particularly cardiac or respiratory conditions.11,12 There are different modalities of inspiratory muscle training, such as inspiratory threshold loading (ITL) and normocapnic hyperpnea (NH). It has been used to increase the strength of inspiratory muscles, reduce dyspnea, and improve exercise capacity, both in association with pulmonary rehabilitation and as a standalone intervention.11,12 Recent evidence suggests that IMT can reduce the activation of type III and IV afferent fibres and, consequently, the development of the IMM, thereby improving tolerance and exercise capacity.13,14 It is well established in the literature that an increase in exercise capacity is associated with improved health status, reduced healthcare utilization, and reduced risk of death in healthy individuals and those with certain diseases.15–18 Activation of IMM may limit exercise tolerance time and exercise capacity in healthy individuals and those with disease.19,20 It is also known that IMT increases exercise capacity, respiratory muscle strength and endurance and may provide an important intervention for improving exercise capacity in persons with problematic IMM.11,12 The effect of IMT on the IMM has not been established, especially in subjects with pulmonary and cardiac disease. It is important to investigate whether IMT has beneficial effects on IMM in different populations, as it could be an intervention used in healthy individuals and patients. This systematic review aims to synthesize evidence about the efficacy of IMT in attenuating IMM and improving exercise capacity in healthy individuals and those with cardiac and respiratory disorders.
Methods
This systematic review was registered in the International Prospective Register of Systematic Reviews (PROSPERO CRD42024526443) and conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) reporting guidelines.21
Eligibility criteria
Eligible articles for this review included randomized controlled Trials (RCTs) and non-RCTs (cross-sectional studies) that investigated the effect of IMT on the IMM in healthy persons or subjects with cardiac or respiratory disease. Studies that included any outcome measures associated with the IMM were eligible for inclusion. These included HR, MAP, and measures of change in blood flow (e.g., oxygenated hemoglobin (O2Hb), deoxygenated hemoglobin (HHb), and total hemoglobin (tHb)). Included studies must use the inspiratory fatigue test to induce the IMM in the subjects.22
The exclusion criteria were studies that did not include a placebo or control group, letters to the editor, case reports, theses and dissertations and were written in languages other than English or Portuguese. The control group should have been composed of individuals with the same condition as the subjects in the treatment group.
Search strategy
A systematic search was conducted in the following databases: MEDLINE/PubMed, SCOPUS, Web of Science and LILACS, through EBSCO from inception through December 15, 2023.
Systematic searches were conducted using the terms “Respiratory muscle training,” “Inspiratory muscle training,” “Breathing exercises,” “Metaboreflex,” “respiratory muscle metaboreflex,” “blood flow,” and “muscle oxygenation.” The search strategy in PubMed and other databases was: “Respiratory muscle training” OR “Inspiratory muscle training” OR “breathing exercises” AND metaboreflex OR respiratory muscle metaboreflex OR blood flow OR muscle oxygenation OR NIRS.
Study selection
The studies identified through the search strategy were exported to the Rayyan system (Rayyan Systems Inc., Cambridge). Subsequently, cross-references and duplicates were excluded independently by two researchers (APSS and DMFA). These researchers also conducted the preliminary selection of studies based on titles and abstracts. Selected studies were read in full to determine those to be included in this review. All the aforementioned steps were carried out independently by two researchers considering the eligibility criteria. Any discrepancies were resolved through meetings to reach a consensus, and a third reviewer was available if needed (TBWL).
Assessment of Methodological Quality
The methodological quality of the studies was assessed independently by two reviewers (TBWL and MGF). For this analysis, the PEDro scale was used, which contains eleven items: eligibility criteria, sample randomization, allocation concealment, baseline group similarity, participant blinding, therapist blinding, assessor blinding, measurement of at least one key outcome obtained in more than 85% of individuals, intention-to-treat analysis, intergroup comparison, measurement of effect size, and treatment variability. The total score ranges from zero to ten points, with higher scores indicating better methodological quality. Item 1 is not considered for calculating the score.23
Data analysis
Data extracted included study characteristics (authors, year, and study design), participant characteristics (age, sex, height, weight, number of participants in each group), intervention characteristics (load, number of repetitions, frequency, duration), outcome measures (HR, MAP, indicators of change in blood flow (e.g., O2Hb, HHb, tHb vascular resistance), and key findings of each study. The data extracted across studies was evaluated for homogeneity. Significant heterogeneity was noted, making meta-analysis not possible. A qualitative synthesis was therefore performed.
Results
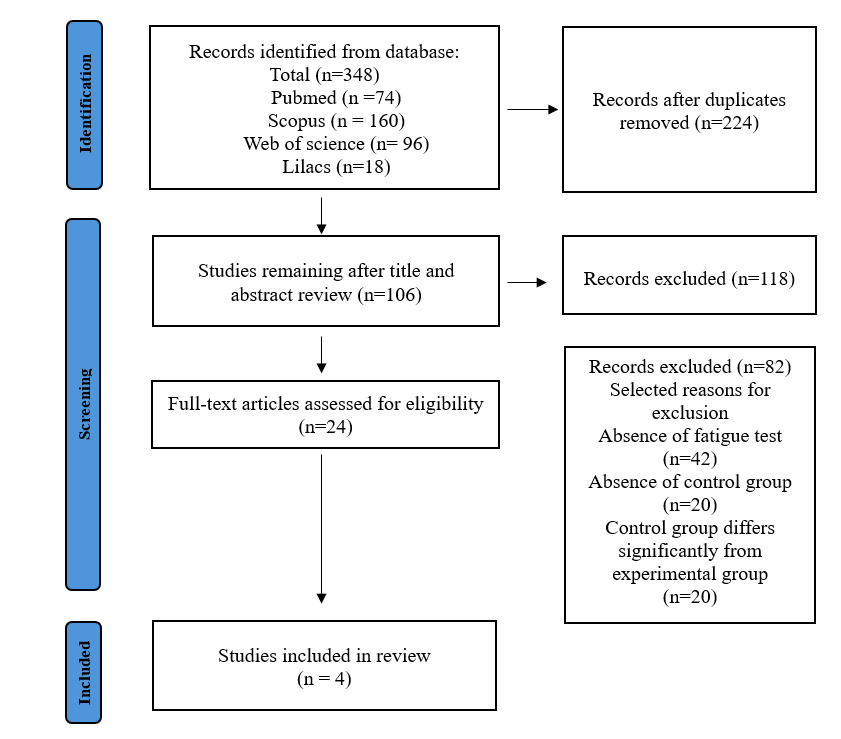
The study selection process is illustrated in Figure 1. Of the 348 studies identified, four met the inclusion criteria for this synthesis. Among these four studies, two were RCTs, and two were non-RCTs.
Study characteristics
The four studies included a total of 76 subjects; one included only women,24 one included only men,13 and two included women and men.14,25 One study was conducted on subjects with heart failure,14 one with soccer athletes,24 and two with healthy subjects.13,25 No studies were found that evaluated the effect of IMT on IMM in patients with respiratory disease. In two studies, the control group underwent sham IMT,13,24 while in the others, the control group did not undergo any type of training14,25 (see Table 1).
IMT Intervention
Of the four studies, three used the Powerbreathe device for IMT,14,24,25 and one used the Powerlung device.13 Regarding the load, three studies used a load of 50% of maximum inspiratory pressure (MIP),13,24,25 and one used a load of 30% of MIP.14 The duration of training varied between 5-8 weeks and 5-6 days per week, with three studies performing training considering the parameter of breaths,13,24,25 ranging from 30-75 breaths per session, and one study performing IMT for 30 minutes per session14 (Table 1).
Outcome Measures
Respiratory muscle strength and Tlim
In all studies, subjects in the experimental group showed an increase in inspiratory muscle strength (MIP) after IMT. Three studies assessed Tlim and observed a significant increase in the total duration time of respiratory fatigue test (Tlim) after the intervention protocol in the experimental group.14,24,25 For example, in the study by Archiza et al.,24 there was a significant increase in Tlim of respiratory fatigue test post-IMT in comparison with pre-IMT ( 204.1 ± 47.1 seconds vs 233.7 ± 61.3 seconds p = 0.002) (see Table 2 in Supplementary Information). In the intergroup comparison, there was no significant difference; however, the experimental group showed a medium effect size, while the control group showed a small effect size (0.74 vs 0.46, respectively).
IMM Measures
Regarding the variables used to assess the IMM, two studies evaluated MAP and HR responses,13,25 while two studies assessed variables related to blood flow such as arterial saturation, O2Hb, HHb, and tHb.14,24 In all studies, IMT was able to attenuate physiological responses associated with IMM. In the studies by Witt et al.13 and Chan et al.,25 there was a significant decrease in MAP and HR in the experimental group during the fatigue test after the IMT protocol in comparison with pre-test. In the study by Witt et al.,13 participants showed an increase of 35% and 17% for HR and MAP, respectively, during the fatigue test. After IMT, this increase was significantly lower during the test, at 27% and 4% for HR and MAP, respectively. In the study by Moreno et al.,14 there was a significant decrease in intercostal muscle and forearm arterial saturation during the respiratory fatigue induced by progressive inspiratory resistive loading. After 8 weeks of training, IMT was associated with attenuation of this reduction of oxygen saturation in the intercostal and forearm muscles during respiratory fatigue. Moreover, the MAP and HR were attenuated during respiratory fatigue test after IMT training (104.8 ± 12.4 vs 99.3 ± 17.3 and 88.4 ± 11.8 vs 81.2 ± 10.6, respectively). Archiza et al.24 observed in their study that there was a significant increase in HHb and a decrease in tHb in the intercostal muscle after IMT, while in the vastus lateralis muscle, there was an increase in O2Hb and tHb (Table 2 in Supplementary Information).
Methodological Quality of Included Studies
The studies showed an average total score of 7 points on the PEDro scale, ranging between 6 and 10 points (see Table 3 in Supplementary Information). A weakness in three studies was the absence of blinding of participants, assessors and/or therapists.
Discussion
The main findings of the present review suggest that IMT may attenuate the IMM in healthy subjects and individuals with heart failure. Additionally, IMT increases inspiratory muscle strength and Tlim. Fatigue is characterized by a decrease in the muscle’s ability to generate force and/or velocity during an activity. Fatigue can limit exercise tolerance in healthy individuals and those with certain diseases.18,26,27 The development of fatigue in the respiratory muscles, particularly in the diaphragm, can activate the IMM, resulting in redirection of blood flow from peripheral muscles, thereby limiting exercise capacity.4–6
There are reports in the literature that respiratory muscles have priority over skeletal muscles in redirecting blood flow during intense exercise.28,29 Dominelli et al.29 conducted a study with healthy subjects undergoing an exercise protocol with increased respiratory work. They observed that when there was an increase in respiratory work, there was simultaneously an increase in blood flow to the respiratory muscles and a decrease in blood flow to skeletal muscles. Furthermore, it was observed that decreased respiratory work with assisted ventilation resulted in decreased blood flow to the respiratory muscles and increased blood flow to the skeletal muscles. They showed that these responses to increased respiratory work were due to activation of the IMM, which could lead to exercise limitation.
IMT is one of the strategies used to minimize the effects of IMM because IMT increases the strength of the respiratory muscles and, consequently, the fatigue resistance of these muscles, according to recent research.30,31 Therefore, by increasing fatigue resistance, the activation of the IMM is attenuated. The increase in fatigue resistance occurs because, with IMT, there is a decrease in anaerobic metabolism and an increase in oxygen consumption.31,32 Hossein Pour et al. conducted an RCT in patients with heart failure and found that 6 weeks of IMT was able to reduce fatigue and dyspnea in these patients.32 This also explains our finding that there is a significant increase in Tlim during the respiratory fatigue test.32 Based on the results of the present review, IMT appears to attenuate IMM in patients with heart failure by increasing fatigue resistance and exercise tolerance. However, further studies are needed in this population to understand the true effects of IMT on IMM.
Due to its vasoconstrictive action, the activation of the IMM will cause an increase in MAP and HR.33,34 The results of this review show that IMT has an attenuating effect on IMM, reducing MAP and HR responses, for example, during the performance of an inspiratory fatigue test or exercise. Furthermore, our results indicate that blood flow to the peripheral muscles is maintained during an activity with increased respiratory workload (inspiratory fatigue test) after weeks of IMT. For example, the result of maintaining blood flow to the peripheral muscles found in the study by Archiza et al. indicates that there was no redirection of blood flow to the respiratory muscles, also demonstrating the attenuation of the IMM.24
The activation of IMM can reduce exercise tolerance in healthy individuals and those with certain diseases. Given this, the strength of the present study is that we demonstrated the efficacy of IMT in attenuating the IMM, identifying it as a potential approach for increasing exercise tolerance in healthy subjects and persons with heart failure. This study has limitations. Specifically, a small number of studies met our inclusion criteria and included a small collective sample size. In addition, some of the outcome data in the articles included in the review were reported as figures, making extraction difficult. The authors were contacted by email, but no responses were received. Therefore, the data were extracted manually using the WebPlotDigitizer website, which allows for figure uploads and numerical data extraction. Two studies did not include randomization and most studies did not incorporate blinding in their study designs. Heterogeneity across studies further limited the ability to draw strong conclusions and make recommendations.
Conclusion
The results of this systematic review suggest that IMT may increase inspiratory muscle strength and attenuate the inspiratory IMM in healthy subjects and those with heart disease. Future randomized, blinded studies are required across a wider range of relevant disease state populations.
Contributors
TBWL and MGF designed research; APSS and DMFA conducted literature search; TBWL and BBSS conducted data extraction and analysis of data; TBWL and MGF conducted manuscript preparation. All authors reviewed manuscript drafts and input corrections. All authors approved the final version of this manuscript.
Funding
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing interests
All authors have completed the ICMJE uniform disclosure form and declare no conflict of interest.
Ethical approval
This systematic review was registered in the International Prospective Register of Systematic Reviews (PROSPERO CRD42024526443) and conducted in accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) reporting guidelines.
AI Statement
The authors confirm no generative AI or AI-assisted technology was used to generate content.
Availability of data and material
Data supporting the findings of this study and additional information are available from the corresponding author upon request.