Introduction
Chronic obstructive pulmonary disease (COPD) significantly impacts the physical activity levels of affected individuals. Physical activity is defined as any body movement produced by skeletal muscles that results in energy expenditure greater than the baseline. This includes a wide range of activities, from those performed during daily living and work-related tasks to recreational activities and structured exercise programs. COPD is a chronic condition characterized by progressive obstruction of pulmonary airflow, leading to symptoms such as dyspnea, cough, and sputum production.1 These symptoms can limit the capacity to engage in both moderate and high-intensity physical activities. Consequently, individuals with COPD often exhibit reduced levels of physical activity compared to the general population, which may have negative consequences for their health and quality of life.2
The limitation in exercise capacity associated with COPD is attributed to various factors, including pulmonary dysfunction, peripheral muscle dysfunction, and the presence of comorbidities such as cardiovascular disease.3 Additionally, fatigue and the sensation of breathlessness experienced during physical activity can act as significant barriers to regular exercise in these individuals. Consequently, many COPD patients tend to adopt a sedentary lifestyle, further contributing to the loss of functional capacity and overall health deterioration.4
It is known that exposure to hypobaric hypoxia associated with high-altitude environments (>2500 m) can have significant effects on people’s physical activity levels.5 The decrease in partial pressure of oxygen (PO2) can lead to a reduction in aerobic capacity and a decline in physical performance.6 This may manifest as quicker fatigue, increased difficulty in breathing, and lower exercise tolerance in individuals with COPD, thereby limiting the ability to maintain physical activity levels comparable to those experienced at sea level or even with levels of individuals without this disease residing at high altitudes.
The reduced level of physical activity in individuals with COPD is associated with a series of adverse consequences, including a higher risk of disease exacerbations, more frequent hospitalizations, and increased mortality.7 Furthermore, physical inactivity may contribute to the deterioration of lung function, decreased muscle strength, and loss of bone mass, further exacerbating disability and reducing the quality of life of these patients. Therefore, the purpose of this research was to compare the levels of physical activity in individuals with COPD versus healthy subjects residing in high-altitude environments.
Physical activity was measured by considering the everyday, routine, and normal activities of individuals in their daily lives. This included the assessment of household chores, commuting, occupational activities, and recreational pursuits that are part of the participants’ daily routines. By considering these common daily activities, we aimed to obtain a more accurate and realistic representation of physical activity levels, avoiding any bias that could arise from a controlled test environment or from physical activities that are not habitual for the participant.
Methods
Study design
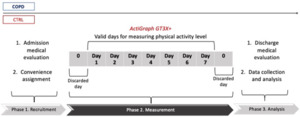
A cross-sectional observational study was conducted on the comparative effects of hypobaric hypoxia on individuals diagnosed with COPD versus those without this disease residing at >2500 m.
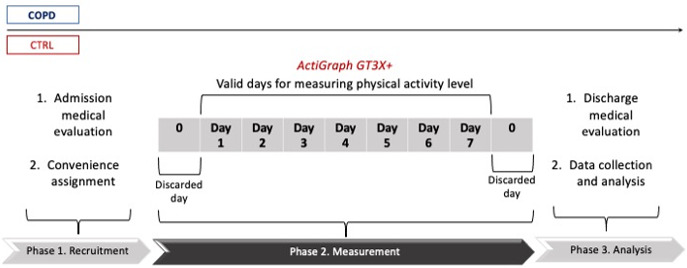
Participants were conveniently assigned to the research groups, considering whether they had COPD or not. The COPD group consisted of individuals diagnosed with COPD, while those without respiratory disease joined the CTRL group (Figure 1).
Participants
The study included adults aged 65 years or older with a medical diagnosis of COPD, classified as GOLD 1 and 2 (A or B) according to the Global Initiative for Chronic Obstructive Lung Disease (GOLD).8 The inclusion criteria were as follows: (i) residing at high altitude (>2500 m) without experiencing changes in altitude in the 24 months prior to the start of the study, (ii) not experiencing disease exacerbations three months before the start of the study, (iii) not requiring oxygen therapy, (iv) being affiliated with a medical insurance system, (v) having signed informed consent.
Individuals were excluded from the study if they met any of the following criteria: (i) having any physical, sensory, cognitive, or psychosocial disability that would limit participation in the physical exercise program, (ii) being diagnosed with cardiac, vascular, renal, or hepatic diseases that could affect the level of physical activity, (iii) being active smokers or being exposed to occupational chemicals that could exacerbate COPD, (iv) actively participating in physical exercise or pulmonary or cardiac rehabilitation programs, (v) being involved in other medical or therapeutic research.
For the CTRL group, inclusion criteria included: (i) individuals aged 65 years or older who have resided at high altitude (>2500 m) for at least 12 months before the start of the research, (ii) not presenting hypoxemia with peripheral oxygen saturation (SpO2) below 92%, (iii) being affiliated with a medical insurance system. Exclusion criteria for this group included: (i) having any disability that restricts the practice of physical activity, (ii) being diagnosed with cardiac, vascular, or renal diseases, (iii) being physically active, recording more than 150 min/week of physical activity, (iv) being an active smoker or being exposed to tobacco smoke.
Outcome variables
Physical activity level was assessed using a triaxial accelerometer ActiGraph GT3X+ (Pensacola, USA, 2011),9 designed to record acceleration with magnitudes ranging from 0.05 to 2.5 g (where g = 9.8 m/s^2), within a frequency range of 0.25 to 2.5 Hz over a period of 60 seconds. This device was secured to each participant’s dominant hip using a belt. Data were collected for a total of nine days, of which seven days were considered valid, excluding the first and last day of measurement. A valid day was defined as one in which the accelerometer was worn continuously for a period of 8 to 10 hours. In data analysis, non-recorded periods were eliminated, defined as a 60-minute interval with a count equal to 0, indicating device non-usage. To determine the level of physical activity, the following outcomes were calculated: (i) Metabolic Equivalent of Task (METs)/hour, (ii) energy expenditure in kcal/hour and kcal/day, (iii) number of steps per day. The physical activity of the subjects was measured according to their everyday activities during the measurement days; therefore, people were instructed to continue with their routine activities in a normal way during the measurement time. The individuals in the study did not participate in any additional or different physical exercise programs beyond what they normally engage in as part of their daily routine. This approach ensured that the data accurately reflected their habitual levels of physical activity without introducing any external or non-routine activities.
Environmental conditions during measurement
The assessment of physical activity level was conducted in a specific geographical and environmental setting with the following characteristics: (i) location: Andean Region, (ii) Altitude: 2,640 m (8,660 feet), (iii) barometric pressure during assessment: 752.1 hPa, (iv) average temperature: 14°C to 22°C (57°F to 71.6°F), (v) relative humidity: 62%.
Ethical aspects
This research adhered to the principles and guidelines established in the Helsinki Declaration and obtained approval from the ethics committee of the Universidad Nacional de Colombia granted on 7 December 2020 and registered with approval number 14-2020. All participants signed an informed consent agreeing to their participation.
Statistical considerations
Taking into account the characteristics of the population object of this research, convenience sampling was developed given that (i) patients with COPD should have stratification of the disease before the start of the study, (ii) control group (CTRL) subjects should not have significant differences around anthropometric conditions, (iii) the study subjects had to be residents at high altitude, (iv) the participants had to have adequate cognitive functions to make adequate use of the accelerometer and for which two education sessions were carried out.
Continuous variables were examined using measures of central tendency (such as mean and median) and dispersion (such as standard deviation and interquartile range), depending on their normal distribution, which was assessed using visual methods (histograms and scatter plots) and statistical tests (Shapiro-Wilk test). Comparison between COPD and CTRL patient groups was conducted using SigmaPlot software (version 12.5, Systat Software, Inc., 2008–2009). Parametric and non-parametric statistical tests were applied based on a priori criteria. Chi-square test was used to compare proportions between groups, while Kruskal-Wallis test was applied for continuous variables. Data are presented as mean ± standard deviation (SD), and p-values indicating significant statistical differences are reported throughout the text, tables, and figures, with significance set at p<0.05.
Results
Six patients diagnosed with confirmed COPD and six individuals without COPD who exhibited similar health characteristics and sociodemographic conditions (all residing at >2500 m) were recruited. (Figure 2). Regarding age, no significant differences are observed between the two groups, with a mean age of 74.0 years for the COPD group and 75.6 years for the control group (p=0.613). However, significant differences are observed in height, with the COPD group being slightly taller on average compared to the control group (161.1 cm vs 151.3 cm, p=0.108). In terms of weight and body mass index (BMI), no significant differences are observed between the two groups, with the COPD group having an average weight of 68.5 kg and a BMI of 26.3 kg·m-2, while the control group has an average weight of 64.2 kg and a BMI of 28.4 kg·m-2 (p=0.556 vs p=0.359). See Table 1.
Regarding pulmonary function tests, significant differences are observed in several parameters between the two groups. The COPD group shows significantly lower forced vital capacity (FVC) and forced expiratory volume in one second (FEV1) compared to the CTRL (p=0.069 vs P=0.089). Additionally, the forced expiratory volume in 1s/forced vital capacity (FEV1/FVC) ratio is significantly lower in the COPD group (p=0.039). Additionally, significant differences are evidenced in the baseline dyspnea score between the two groups, with the COPD group experiencing a higher dyspnea score compared to the CTRL group (3.6 vs 1.6, p=0.002). Furthermore, significant differences are found in pulse arterial oxygen saturation (SpO2) and breath frequency (BF), with lower SpO2 values and higher BF in the COPD group compared to the CTRL group (p<0.001 and p=0.030).
Physical activity level
Daily calorie expenditure associated with physical activity was slightly decreased in patients diagnosed with COPD compared to the CTRL group, with a percentage difference of 3.1% (Kcal/day: COPD 197.84 ± 85.4 vs CTRL 191.94 ± 105.9. p=0.398). Regarding calorie expenditure per hour, a significant difference was observed between both groups, showing that the COPD group had a 61.32% lower hourly calorie consumption rate compared to the control group (Kcal/Hour: COPD 8.92 ± 5.4 vs CTRL 14.49 ± 16.7. p=0.018)
In relation to METs/hour, a 9.64% difference was found between the COPD group and the control group, with lower METs recorded in COPD patients (METs/hour: COPD 1.25 ± 0.1 vs CTRL 1.24 ± 0.25. p=0.025). Finally, quantification of physical activity level through the number of steps per day showed a significant difference of 139.41% between the groups, with an average of 2312 fewer steps in the COPD patient group (steps/hour: COPD 1658.50 ± 252.05 vs CTRL 3970.75 ± 397.19. p=0.001).
Regarding the results separated down by day, it is evident that the analysis of daily caloric expenditure (Kcal/day) reveals notable differences between the groups over the week. During this period, patients with COPD exhibit a range of 145.6 to 229.7 kcal/day, while the control group shows a broader spectrum, fluctuating between 135.05 and 235.9 kcal/day. Regarding hourly caloric expenditure (Kcal/hour), marked fluctuations are observed in both sets of participants over the seven-day study. Patients with COPD display a range of 6.27 to 12.81 kcal/hour, while the control group has a range of 7.76 to 16.85 kcal/hour, indicating variability in physical activity patterns during the observation period (Figure 3).
The METs per hour rate (METs/hour) also exhibits significant variations both between the groups and over the study period. Patients with COPD register a METs per hour rate ranging from 1.198 to 1.293, while the control group shows values ranging from 1.157 to 1.312, highlighting differences in the relative intensity of physical activity performed. Finally, the analysis of the number of steps per day (steps/day) reveals a considerable disparity in levels of physical activity between patients with COPD and the control group over the week. Patients with COPD show a range of 922.28 to 2166.48 steps/day, while the control group records a broader range, from 3413.67 to 4993.13 steps/day, reflecting differences in mobility and the level of physical activity between the two groups (Figure 3).
Discussion
The assessment of physical activity level through daily step counts reveals a marked disparity between the groups, with COPD-diagnosed patients showing an average of 2312 fewer steps than the control group. When contrasting our step count data with previous studies by Carvalho da Silva et al. (Steps/1Day 3066),4 Albarriti et al. (Steps/1Day 4095),2 Wats et al. (Steps/1Day 7990 ± 3370,)10 and Troosters et al. (Steps/1Day 5584 ± 3360,)11 This disparity could be attributed to the coexistence of hypoxemia associated with structural and functional lung damage derived from COPD, along with exposure to altitude hypoxia due to their residence in high-altitude regions.7 The observed difference between the study groups suggests a notable decrease in daily physical activity in COPD patients, a phenomenon that may be related to respiratory difficulty and fatigue experienced during daily activities.
Although no significant difference was found in quantifying daily caloric expenditure, a significant difference was found in hourly caloric expenditure between the two groups; this may be associated with the fact that daily caloric expenditure can be influenced by a wide range of physical activities performed throughout the day.12 Thus, while COPD patients may experience limitations in certain physical activities due to their medical condition, they may compensate with other lower-intensity activities that may not reflect in a significant difference in daily caloric expenditure. Conversely, hourly caloric expenditure may be more directly affected by limited respiratory capacity and fatigue associated with COPD.13 Activities requiring more intense physical effort may result in greater respiratory difficulty for COPD patients, limiting their ability to maintain a steady pace of physical activity,2 and thus reducing their hourly caloric expenditure.
Regarding METs, COPD patients exhibit a lower number of achieved METs/hour, suggesting reduced capacity to perform physical activity at a higher metabolic level in these individuals. The reduction in METs is associated with physiological and metabolic factors present in COPD patients, such as: (i) decreased metabolic efficiency and cellular oxidative capacity, likely stemming from lower synthesis of oxidative enzymes in muscle tissue,14 (ii) increased mitochondrial degradation, which could be linked to the chronic inflammatory response characteristic of COPD, as well as disuse due to physical inactivity,15 (iii). reduction in the proportion of capillarization per muscle area and in the proportion of slow oxidative muscle fibres (Slow Oxidative: SO),16 which could influence the capacity of COPD patients to maintain optimal levels of physical activity in the long term,14 (iv) exposure to hypobaric hypoxia imposes additional stress on the respiratory system, increasing disease exacerbations and typical respiratory symptoms in people with COPD.17
All participants in this research do not meet the minimum requirements to be physically active (regardless of whether they have a diagnosis of COPD), an aspect that may be associated with the effects of hypobaric hypoxia on functional fitness and physical independence. It is known that lower partial pressure of oxygen in the air can lead to a decrease in exercise capacity and an increase in fatigue18; likewise, physiological stress caused by hypobaric hypoxia along with adverse climatic conditions may reduce motivation to engage in intense physical activities.
These findings underscore the importance of considering the impact of COPD on physical activity and caloric expenditure in patients. The reduction in the ability to engage in physical activity observed in COPD patients could have significant implications for their health and quality of life, highlighting the need for interventions that promote physical activity tailored to the limitations of these patients.
Finally, although the sample size in this scientific study is small, these results are novel and innovative, considering that the number of investigations into the effects of hypobaric hypoxia on the level of physical activity in people with COPD is limited. Thus, the results of this study can serve as a starting point for future larger and more comprehensive studies in the same field, providing a solid foundation for the exploration and broad understanding of the relationship between respiratory disease, altitude hypoxia, and physical activity.
Conclusion
These results suggest that patients diagnosed with COPD may exhibit lower levels of physical activity compared to healthy individuals when residing in hypobaric hypoxia environments. COPD subjects may have up to 61% less daily caloric expenditure, 3% less hourly metabolic expenditure, and approximately 139% less daily physical activity measured in terms of steps taken. We believe that this low level of physical activity observed in individuals with COPD, particularly those residing at high altitudes, could be a contributing factor to the functional limitations and deterioration in quality of life associated with this disease.
Acknowledgment
We are grateful for the contribution of Edgar Cristáncho Mejía and Erica Mancera Soto.
Funding
This research was funded by the Universidad Nacional de Colombia, through the “Call for the support of research projects and artistic creation of the Bogotá campus – 2019, code HERMES, 47970”. The funding organization was not involved in the investigation.
Conflict of interest
The author completed the ICMJE uniform disclosure form and declares no conflict of interest.
Ethical Approval
Approval was granted by Universidad Nacional de Colombia granted on 7 December 2020 and registered with approval number 14-2020. Research registration: NCT04955977 [WHO ICRTP].
Statement on AI
During the development of this article, the researcher utilized the artificial intelligence tool ChatGPT 4.0, developed by OpenAI (San Francisco, California, USA, 2020), to enhance the writing and clarity of the text, particularly in the introduction. This was undertaken to refine the use of the English language, given that the primary author is not a native English speaker. Subsequently, the author reviewed and adjusted the resulting content, assuming full responsibility for its final publication.